Northern Ireland's health challenges
- Published
- comments

Belfast's Royal Victoria hospital has been at the front line of a challenging few years for the NHS
The NHS in Northern Ireland has not had a good press in recent years.
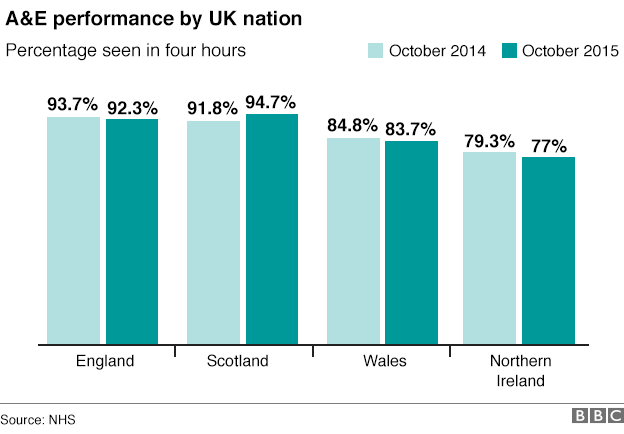
Accident and emergency waiting times for patients have lagged behind other parts of the UK.
Two years ago, a major hospital in Belfast, Royal Victoria, was said to be "at breaking point", as a backlog of patients built up and a major incident was declared.
But, even with the latest provisional figures showing a decline in A&E performance, there is a determination among clinicians and nursing staff to draw a line and build a level of service to be proud of.
There is evidence of a change of mood with the opening in August of an emergency department at Royal Victoria, part of a new £150m critical care facility.
Doctors, bruised by the turmoil in the 2013-14 winter, have developed new ways of working, designed to speed the flow of patients through the system.
It's early days, but there are some encouraging signs - in recent months, there has been a 10% year-on-year increase in the number of patients treated or assessed within four hours.
The most recent data for November, though, shows an increase of five percentage points year-on-year.
The hospital points out it has dramatically reduced the number waiting 12 hours or more.

New facilities being built at the Royal Victoria
A key policy at the Royal Victoria is putting senior clinicians close to the "front door" of the emergency department.
Their task is to quickly triage patients and send them through different treatment streams.

The NHS in winter: Want to know more?

Special report page:, external For the latest news, analysis and video
Analysis: The lost beds problem
Winter across the UK: A guide to how the NHS is coping
Video: Why hospitals are under so much pressure
Video: How a hospital can grind to a halt

The idea is to avoid a build-up of people waiting in reception.
Badly injured or sick patients are dispatched through the system in the normal way, but a more sophisticated approach has been developed for those who are less seriously ill.
A critical-assessment unit next to the emergency department receives patients, with the aim of dealing with their medical needs within the day.
This could involve an initial appraisal and then sending a patient home for the night with an appointment booked the next day.
Known as a "virtual ward", the idea is to carry out treatment without patients needing overnight stays, so reducing pressure on bed occupancy.
Specialist equipment is made available to this unit, allowing doctors to order scans and other procedures to accelerate the patient's progress.
Royal Victoria and other emergency departments are facing deep-rooted pressures.
Northern Ireland does not have a 111 or NHS Direct helpline to guide patients, where appropriate, away from A&E towards other forms of treatment closer to home.
And there are only a few minor injuries clinics to take the pressure off the major hospitals.
The Northern Ireland Health and Social Care Board has announced measures to boost GP out-of-hours services and promote alternatives to turning up at A&E.
The NHS has to cope with long-standing health problems in some areas, including mental health, which can be linked to economic decline and deprivation.
The integration of health and social care offers Northern Ireland the opportunity to tackle major problems common to all parts of the United Kingdom.
Problems caring for the elderly at home and in their local communities have left most UK hospitals struggling to discharge patients and free up beds for new patients to occupy.
Southern Health and Social Care Trust in Northern Ireland is pioneering consultant-led care of the elderly in the community, offering, in effect, hospital care in a patient's own home.
The service aims to treat at home patients with a wider range of acute illnesses.
In its first year, the pilot service has prevented about 440 hospital admissions.
With 1.8 million people, it will always be a challenge for Northern Ireland to sustain a full range of NHS services and specialist care.
There is clearly a will to rise to that challenge, but no-one is denying the task may get harder with rising attendances at hospitals, an ageing population and complex health needs.