Winter pressures: A detailed look at how the NHS is coping
- Published
Winter is the busiest time of year for the NHS. The cold weather, coupled with illnesses such as flu, mean hospitals tend to see a rise in the number of frail and vulnerable patients.
So throughout the winter, the BBC will be keeping an eye on how the health service is performing.
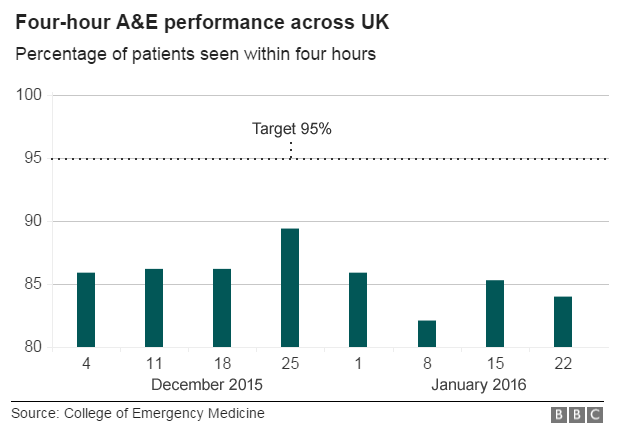
For the most straightforward and up-to-date overview of what is happening, the Royal College of Emergency Medicine's weekly snapshot of more than 40 major NHS trusts - one in five of the total - is the best source.
It suggests the four-hour target to treat or admit patients is proving difficult to achieve - hospitals are meant to see 95% of patients in that timeframe.
To find out more about why hospitals are under so much pressure have a watch of the video below.
Nick Triggle explains the various factors behind the mounting problems the NHS is facing
So what else do we know? Well, the picture is complicated because the way official data is collected varies in different parts of the UK.
With the exception of Scotland, the figures provided by the NHS lag behind the Royal College of Emergency Medicine's data by between four and six weeks.
Nonetheless, we can still draw out an interesting picture of what is happening.

England
Unlike previous years, the NHS is not publishing weekly data on how it is performing against the four-hour target.
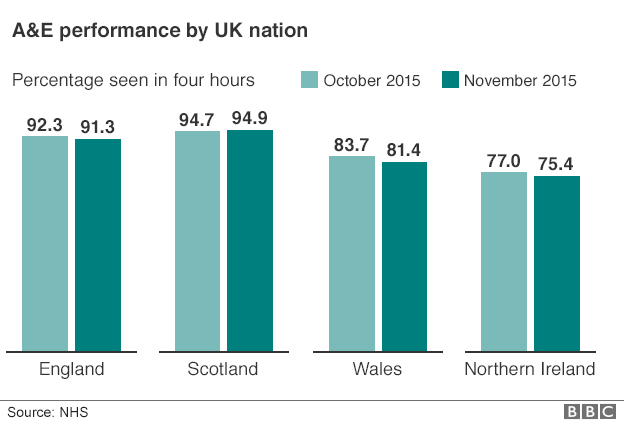
Instead this is now being released monthly. The latest figures for November showed 91.3% of patients were seen in four hours. This sort of performance is normally seen in the depths of winter.
Other key targets are also being missed.
The last time ambulances hit their target to answer 75% of the most serious 999 calls in eight minutes was May.
One of the key cancer targets - the 62-day target for treatment to start - has not been hit for over a year.
The NHS 111 phone service is missing its target to answer 95% of calls within 60 seconds.
As winter has progressed there are signs the difficulties have increased. In the past weeks there have been reports of hospitals going on black alert - this is an indication for the reset of the system that a site is under strain and struggling to cope. A hospital on black alert may be taking extraordinary steps such as cancelling non-emergency operations and re-deploying staff.
Hospitals seem to be having a particular problem with discharging patients. The most vulnerable patients - mainly elderly, frail people - need to have support in place in the community from council care teams and community nursing before they can be released, even though they may be medically fit to leave hospital.
When this cannot be found, the patients are classed as a delayed discharge. The number of delays has now reached the highest level since record-keeping began in 2010. Reports suggest some hospitals may have a fifth of their beds taken up by patients who should not be there.
Analysis: A 'good' Christmas for the NHS - but what's to come?

Northern Ireland
Out of the four UK nations, Northern Ireland is doing the worst. The graph below shows its performance, according to the official statistics, against the rest of the UK nations for November - the latest month for which there is complete data.
Northern Ireland also provides data on 12-hour waits. A total of 288 patients waited this long, double the number 12 months previously.
By the start of 2016 health chiefs were warning that the system was under severe pressure and patients should only head to A&E in an emergency.

Wales
Wales has experienced its share of problems too. A&E performance is better than in Northern Ireland, but still some way short of what is being achieved in England and Scotland.
In November the official figures showed just over 81% of patients were seen in four hours. By early January reports were emerging of "unprecedented demands" being placed on hospitals and the Royal College of Emergency Medicine said A&Es were "on the edge".
But it is not just A&E units that are struggling. Like England, other parts of the system are under pressure.
The number of people on waiting lists for routine operations, such as knee and hip replacements, has been growing. Latest figures show there are nearly 450,000 - 10% higher than it was three years ago.
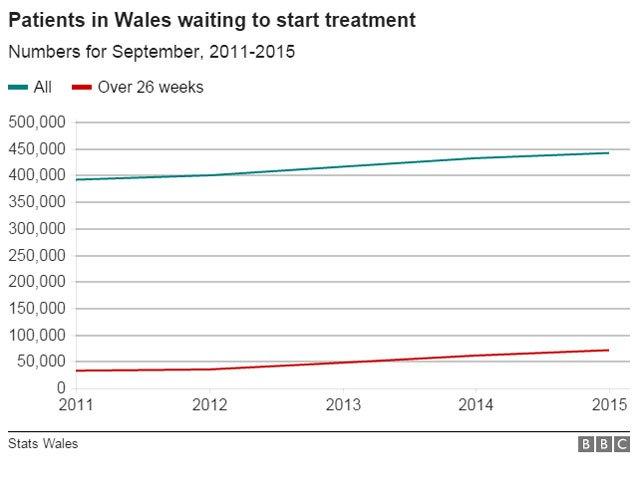
The Royal College of Surgeons recently described this as "unacceptable" and urged ministers to address the problems.
But Wales has unveiled plans to help it cope including a push on reducing admissions and delays discharging patients.

Scotland
Out of all the four nations, Scotland is arguably in the best position. It is the only health service that is actually doing better than last year.
The latest monthly performance figure shows 94.9% of patients were seen in four hours.
And this position seems to be holding up. Scotland provides up-to-date information on the performance of the 30 busiest hospitals on a weekly basis. The data over Christmas shows performance was actually just above the 96% mark although by early January there were signs winter was starting to hit performance.
Councils and the NHS have been encouraged to pool budgets and a number of places have opened up intermediate care beds.
This appears to have led to a reduction in the delayed discharges that have proved so problematic in England.
In Glasgow, for example, about 100 beds have been opened for this purpose over the past year.
The impact has been staggering. On the first Monday of December last winter 117 hospital patients had been waiting more than 72 hours to be discharged. This winter there were 27.
- Published27 November 2015

- Published27 November 2015

- Published25 November 2015

- Published12 November 2015

- Published12 November 2015
- Published9 October 2015

- Published9 October 2015