Pregnant women with epilepsy 'need specialist care'
- Published

Pregnant women with epilepsy should be treated by a specialist healthcare team to prevent unnecessary deaths, according to new national guidelines.
Produced by the Royal College of Obstetricians and Gynaecologists, the guidelines recommend women seek advice well before pregnancy on their care.
Managing seizure control, tiredness and risks linked to some epilepsy medicines can make pregnancy a difficult time.
Epilepsy Action said the guidance would help women make informed decisions.
Around 2,500 infants are estimated to be born to women with epilepsy every year in the UK.
Early advice
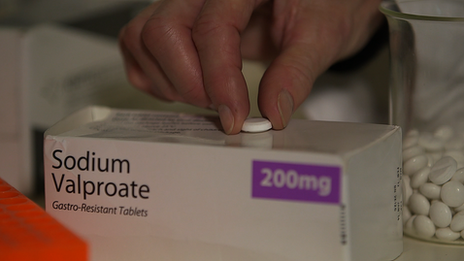
But there are risks to the health of unborn babies from taking some anti-epileptic drugs during pregnancy, particularly sodium valproate.
Some women stop taking their medication or cut down, which can make seizures worse and increase the risk of harm to mother and baby.
However, the guidance says "most mothers have normal healthy babies", but women with epilepsy should be informed that the risk to the foetus is dependent on the type, number and doses of drug they take.
These RCOG guidelines, external, for GPs, midwives, consultants and women with the condition, say women should:
seek advice from their GP before conception
be given the lowest effective dose of the most appropriate epilepsy medication
take a higher dose of folic acid to reduce the risk of spinal defects in their baby
give birth in a consultant-led unit if at risk of seizures during labour
receive support after the birth to minimise the risk of seizures from exhaustion and stress

What is epilepsy?
It's a condition that affects the brain, leading to epileptic seizures.
A seizure happens when there is a sudden burst of intense electrical activity in the brain. This causes a temporary disruption to the way the brain normally works.
There are many different types of seizure. During the more serious ones, the person can lose awareness, go stiff, fall to the floor and the body can jerk.
Some types of epilepsy last for a limited time and the person eventually stops having seizures. But for many people epilepsy is a life-long condition.

Shakila Thangaratinam, lead author of the guidelines and professor of maternal and perinatal health at Barts and the London School of Medicine and Dentistry, said the right care before, during and after pregnancy was important.
"Women with epilepsy require multi-disciplinary care throughout their pregnancy, and healthcare professionals need to be aware of the small but significant increase in risks.
"While most women who have epilepsy remain free of seizures throughout their pregnancy, some may have more seizures if they are pregnant.
"It is important that these women receive pre-conception counselling, meet with an epilepsy specialist, and are monitored closely for seizure risk factors."
Close monitoring
Simon Wigglesworth, deputy chief executive at Epilepsy Action, said he was delighted to see the guidance published.
"This ensures that they are able to make informed decisions about all aspects of their health and wellbeing, as well as that of their baby."
Louise Silverton, director for midwifery at the Royal College of Midwives, also welcomed the guidance.
"It is vital we remember that women with epilepsy are classified as high risk during their pregnancy, often they require more monitoring and specialist care during the course of their pregnancy. However, the majority of women with epilepsy will give birth safely."
Experts say the risk of death is 10 times greater in pregnant women with epilepsy compared with those without the condition.
Between 2009 and 2013, 21 women died during pregnancy as a result of epilepsy - and in most of those cases their seizures were found to be poorly controlled.
- Published25 February 2013
- Published28 September 2012