Game-changing moment for the NHS in England?
- Published

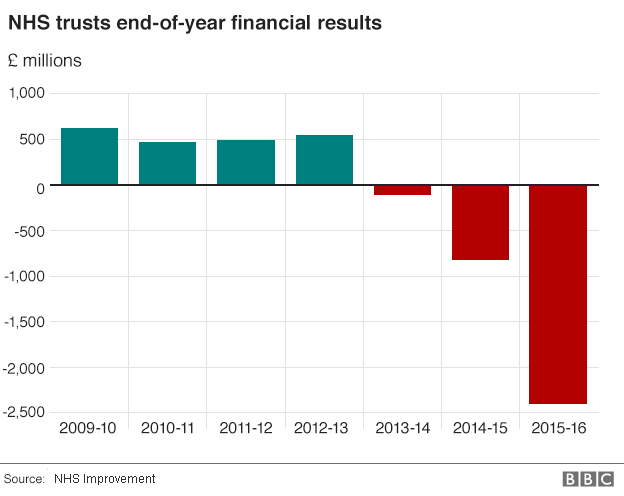
In the final hours of the parliamentary session, there were some fascinating revelations about the state of NHS finances in England.
The Department of Health annual report confirmed how close it had come to breaking Whitehall rules, and there was an amber-light warning from the spending watchdog.
With that, came a plan from NHS England to get the finances under control, which involves a relaxation of the patient-care target regime.
This feels like a game-changing moment for the service.
NHS cash crisis: Hospitals allowed to miss targets
Patients 'could suffer' as NHS trusts bust budgets
Is enough being spent on the NHS?
The reasons for financial pressures are well known, including increasing patient demand, with more complex conditions and staff shortages causing spiralling agency bills.
There have been warnings for some time from health think tanks that the only way for hospitals to stay within budgets is to let waiting times grow and standards slip.
The latest announcement has heightened their suspicions.

Targets and fines: How they work
Accident and emergency: 95% of patients are meant to be dealt with within four hours. When the numbers waiting longer than this exceed that threshold hospitals are fined £120 per patient. The fines are capped so that once it drops below 85%, no more penalties are imposed.
Routine operations: 92% of patients are meant to start treatment within 18 weeks. When the numbers waiting longer than this exceed that threshold hospitals are fined £400 per patient. The fines are capped so that once it drops below 90%, no more penalties are imposed.
Cancer: Hospitals are meant to start treatment on patients who receive an urgent referral by a GP within 62 days for 85% of patients. Fines of £1,000 per patient are levied when patients wait longer. There is no cap.

The National Audit Office pulled no punches in its assessment of the Department of Health accounts for 2015-16.
It said that officials had only managed to keep to the spending limit agreed by Parliament because of an unexpected £400m National Insurance windfall.
The Treasury was not informed because of an "administrative error".
The NAO notes that the switching of resources from capital to revenue budgets "means that long-term investment plans have been set aside for the short-term goal of meeting day-to-day spending".
Its conclusion is blunt: the health service is "still some way from implementing a plan to put the NHS finances in England on a sustainable footing".
And remember, the 2015-16 year had seen the much hailed "£2bn boost for the NHS" announced by the then Chancellor, George Osborne, before the general election.
The head of NHS England Simon Stevens argued in a BBC interview that although things had been difficult in the past financial year, there was now a plan to reduce burgeoning trust deficits.
A "special measures" regime will see some trusts under a tight rein for controlling spending.
Agreed budget totals have been set, and hospitals and other organisations will be obliged to stick to them.
There will no longer be fines for missing targets for A&E, elective procedures and cancer treatment.
Instead, there will be financial incentives to coax trusts to improve.
This represents a big change in the target-driven approach to maximising health service performance.
So what does all this mean for patients?
It's hard to see how NHS performance will improve any time soon, and health service leaders will have to work hard to convince people that relaxing the target regime will not leader to longer waiting times.
The Patients' Association described the situation as "disastrous".
Nigel Edwards, chief executive of the Nuffield Trust think tank, did not beat about the bush.
"The next steps could be a series of brutal service reductions and bed closures - which will shock an unprepared public," he said.
These are undoubtedly difficult times for the NHS.
Simon Stevens and his colleagues at the regulator NHS Improvement understandably feel the need to get a firm grip on the finances.
But they are treading a fine line that could result in increasing frustration for patients.
The demands for more government money will increase in volume.
- Published21 July 2016
