Seven-day NHS 'impossible under current funding levels'
- Published

A seven-day NHS is "impossible" to achieve with the current funding and staffing levels, the chief executive of NHS Providers says.
Chris Hopson told the BBC's Andrew Marr programme that "something has to give" and there should be a debate about which services to sacrifice "rather than pretend the gap doesn't exist".
Figures show waiting times and delayed hospital discharges at record levels.
The government says it is giving NHS England the £10bn it asked for.
Health Secretary Jeremy Hunt has called for a "seven-day NHS" since 2015 after his department concluded, external that there was a "clear link between poorer outcomes for patients and uneven service provision at the weekend".
'Relative risk'
Introducing a seven-day NHS also formed part of the Conservative Party's manifesto, and its based on data which suggests that patients are 16% more likely to die if they are admitted on a Sunday compared with a Wednesday.
However, the reasons for this have been contested, and medical professionals agree that people who arrive in hospitals at weekends tend to be sicker than those who do so during the week.
Chief Executive of NHS providers Chris Hopson: NHS 'under greatest pressure in a generation'.
NHS Providers, the organisation that represents hospitals in England, says unless urgent funding is provided it will have to cut staff, bring in charges or introduce "draconian rationing" of treatment, for example, of non-urgent operations.
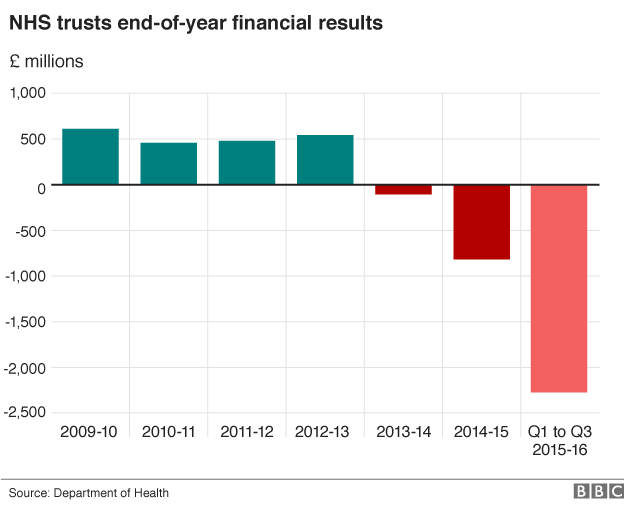
It highlights that 80% of England's acute hospitals are in financial deficit, compared with 5% three years ago - while missed A&E waiting time targets have risen from 10% to 90%.
Is enough being spent on the NHS?
NHS weekend: 7-day services explained
Seven-day NHS - claims and counter claims
Mr Hopson said the NHS was under the "greatest pressure that we've been for a generation".
He added: "Jeremy Hunt and others have made a very strong case for seven-day services, but it seems to us it's impossible on the current level of staff and the current money we have available."

Analysis

By Nick Triggle, BBC health correspondent
On almost every measure, the last few years has seen a decline in performance in the NHS in England (although the rest of the UK is not immune to this either).
That should not come as a surprise. Overall the last five years has seen the tightest financial settlement in the history of the NHS.
To stem the decline, ministers agreed 2016-17 would see the biggest cash injection - nearly 4% above inflation - since the Labour years.
The jury is still out over whether that will have an impact. But even if it does the following years will see much smaller rises so the fear is any respite will only be short-term.
Yes there is a productivity drive, but it is the most ambitious one ever set. Most observers believe it would be amazing if it was achieved in full.
And that's before the seven-day initiative is even factored in.
So that leaves the government with three choices: Put more money in, accept a further decline in standards or cut back on what the NHS does. None of them are particularly palatable for the government.

Mr Hopson also said the numbers of hospitals in deficit, and the missed waiting times for A&E, showed there was "clearly a system-level problem - it's not a problem of poor management".
People on the front line in the NHS were saying that they "cannot provide the right quality of care, and meet the performance standards, on the money that's available".
Mr Hopson said he wanted to see the seven-day NHS idea abandoned, and more money put into the NHS through general taxation.
But he added that the NHS's chairs and chief executives were "absolutely signed up" to deliver "stretching savings targets, and stretching productivity".
His warning comes days before the Commons Health Select Committee will decide whether to launch a special inquiry into the state of the NHS in England and two months before the government announces its spending plans in the Autumn Statement.
In July more than 50 hospitals in England were given the go-ahead to miss key waiting time targets this year to help ease their financial problems.
Fines for missing targets in A&E, cancer and routine operations have also been scrapped altogether and a new failure regime is being set up for the worst-performing trusts.
The Vale of York trust considered suspending non-urgent treatment for obese patients and smokers for a year in order to ease financial pressures before bosses intervened.
Home Secretary Amber Rudd rejected Mr Hopson's suggestion that a seven-day NHS was impossible to deliver.
"The health secretary and the government consulted with [NHS Chief Executive] Simon Stevens and asked him about what scale of money was necessary - we've delivered on that money," she told Andrew Marr.
UK funding
But Chris Ham, chief executive of the King's Fund think tank, said the government should heed "warning signs" and not wait for a "full scale crisis to develop".
He added: "It is simply not realistic to expect hard-pressed staff to deliver new commitments like seven-day services while also meeting waiting time targets and reducing financial deficits."
Diane Abbott MP, shadow health secretary, said: "Years of Tory underfunding of the NHS has made it is impossible to provide the right quality of service and meet performance targets.
"The government needs to properly fund the NHS if it is to function properly. This is what Labour would do."
In June, Northern Ireland Finance Minister Máirtín Ó Muilleoir said its health service was to receive an extra £72m to help deal with pressures in the service, bringing the total additional funding for health to £200m in 2016-17.
Scotland's First Minister Nicola Sturgeon announced in June that minimum staffing levels in Scotland's NHS are to be enshrined in law.
And Welsh Assembly Finance Minister Jane Hutt announced last December that the NHS would be getting a net boost of £278m under the Welsh government's spending plans for 2016-17.
- Published25 February 2016
- Published21 July 2016

- Published13 May 2016

- Published14 January 2016

- Published9 February 2016
