Good bacteria: Why I put my poo in the post
- Published
"Good bacteria" - what are they, will they make me healthy and how do I get some?
To find out I took the unusual , and rather disgusting, step of donating my poo to science.
Microbes live on, and in, all of us and they even outnumber our own human cells.
But their favourite spot - and where they live in incredible numbers - is our digestive system.
That's why I posted my faeces to the British Gut Project, external for analysis.
"You're not exactly average, but you're not way off the chart either," its director, Prof Tim Spector, tells me.
The bacteria in my stool were studied not with a microscope, but with powerful tools to identify them by their genetic code.
It showed I was missing whole groups of bacteria. One area of concern was my Firmicutes, as I had fewer than other people.
"They're generally the ones that have your beneficial microbes in it, suggesting you've got less general diversity than the average person," Prof Spector told me.
"The less diversity you have, the less healthy your gut. It's not a good thing."
A deeper trawl uncovered I had high levels of Akkermansia, which "is generally seen in people who are lean and healthy". But I was also harbouring those linked with inflammation.
There is growing interest in understanding the health consequences of the microbiome.

The microbiome
You're more microbe than human - if you count all the cells in your body, only 43% are human
The rest is our microbiome and includes bacteria, viruses, fungi and single-celled archaea.
The human genome - the full set of genetic instructions for a human being - is made up of 20,000 instructions called genes.
But add all the genes in our microbiome together and the figure comes out between 2 million and 20 million microbial genes.
It's known as The Second Genome and is linked to diseases including allergy, obesity, inflammatory bowel disease, Parkinson's, whether cancer drugs work and even depression and autism.

Are "bad" bacteria or too few of the good ones causing disease?
Prof Spector argues the microbiome is the "most important, exciting thing in medicine today" and that "diversity" - having as wide a range of different species as possible - is key.
Clearly I could do with some improvement. So here are the tips I picked up along the way while making The Second Genome series.
Fibre, fibre... fibre
Researchers Eric Alm and Lawrence David have some of the most studied microbiomes on the planet.
They spent a year analysing 548 of their stool samples.
Lawrence David, an assistant professor at the Duke Center for Genomic and Computational Biology, said diet had the biggest influence on the microbiome - and one thing was especially effective.
He says: "One of the leading sets of molecules that people are getting excited about have to do with plants, specifically fibre.
"It's what at least some bacteria in the gut love to eat."
He says plant fibre is likely to benefit most people's microbiome, though he admits the study has just made him feel more guilty about the food he eats.

"I still eat hamburgers and chicken nuggets," he confides.
Fermented foods 'the future'
Fibre is a prebiotic, providing fuel for the microbes that are in our digestive system.
But Dr Paul Cotter, who I met at the University of Cork, is concerned we're not introducing enough new microbes into our bodies.
He told me: "An awful lot of what we eat now are foods within tins or with an awful lot of shelf-life and they have a long shelf-life simply because there are very few, or not any, microbes within them."
His field is fermented foods that bacteria have gone to town on before you eat them.
Fermented foods include well-known favourites, such as cheese and yoghurt, but also the milk drink kefir, a tea called kumbucha and certain cabbage dishes, such as sauerkraut or the Korean kimchi.
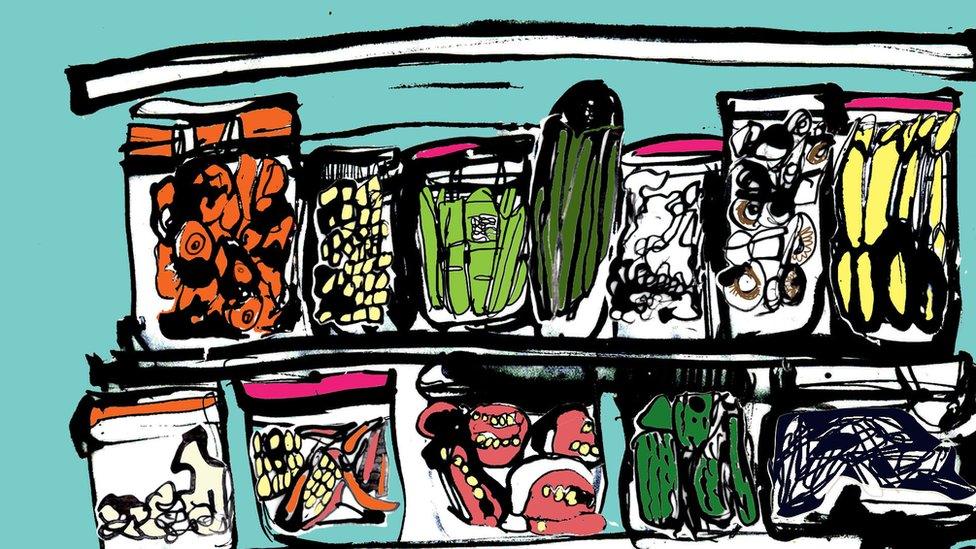
Dr Cotter says most people should be thinking of adding fermented foods to their diet as the microbes in them help calibrate the immune system.
He said: "If you're already healthy, the way to go is consume fermented food rather than going for a particular probiotic, external" - although studies have shown some probiotic products can help prevent necrotising enterocolitis, external and diarrhoea, external in some cases.

Listen to The Second Genome on BBC Radio 4.
The next episode airs 11:00 BST Tuesday April 17, repeated 21:00 BST Monday April 23 and on the BBC iPlayer

Fibre and fermented foods are a good rule of thumb, but there is no guarantee they will work for everyone.
Everybody's microbiome is unique, so the spectacular biology they are performing in the gut varies from one person to the next.
Eric Alm, of serial-faeces-monitoring fame and the co-director of the Center for Microbiome Informatics and Therapeutics at MIT, argues dietary advice will have to be more personalised in the future.
He says: "One thing that we're learning is, based on the microbiome, different people may need to consume different diets in order to get the same effect."
Chain reaction
He has studied what different people's microbiomes do with different dietary fibres.
Broadly, fibres are broken down into chemicals called short chain fatty acids.
They can be absorbed by the intestines and have effects throughout the body. It is one of the ways the microbiome is thought to influence our health.
Prof Alm's work showed some people's microbiome was very good at making short chain fatty acids from a dietary fibre called pectin, which is found in apples and oranges.
Other people's needed inulin (found in leeks, asparagus and onions) to make the same short chain fatty acids.
Prof Alm says: "You can imagine a future where if you needed to increase the levels of butyrate (a type of short chain fatty acid) production in the gut, which some people think might be advantageous for diseases like inflammatory bowel disease, you might sequence your microbiome first.
"[Then] figure out what species are there, then take a prebiotic or dietary fibre supplement that matched the microbes you have to produce butyrate."
Follow James on Twitter., external
Illustrations: Katie Horwich