Doctors used as 'guinea pigs' in opioid painkiller promotion
- Published

Common opioids include morphine, tramadol and fentanyl
"Everybody said, 'It's fantastic going to New York. It's like being on a film set.' So, that was very exciting for me."
Dr Cathy Stannard was one of a group of UK pain specialists flown to New York in the early 2000s.
They had stayed in a smart hotel, eaten in upscale restaurants and attended Broadway shows, she told BBC Radio 4's File on Four programme - all courtesy of a pharmaceutical company.
The trip had been presented as an educational package, an opportunity to meet "international thought leaders" from the world of pain management, she said.
She had known the company footing the bill manufactured opioid painkillers.
But she had not known that, around that time, some pharmaceutical companies would monitor the prescribing rates of the individual doctors who attended such paid-for trips, deliberately targeting those they thought they could influence.
'Promote prescribing'
In a 2007 editorial in the British Pain Society newsletter, Dr Ed Charlton, the organisation's president at the time, flagged up the conflict of interest this kind of hospitality created.
A "jubilant marketing manager" had told an annual conference most of the doctors "started prescribing more of the product", Dr Charlton wrote.
Dr Stannard now regrets her visit to New York.
"I feel very ashamed of that," she said.
"I was just a guinea pig to promote the prescribing of a class of drug."
Hospitality visits
Napp Pharmaceutical - the company that paid for the trip - told BBC News they had always supported the exchange of ideas and best practice between clinicians.
And the objective of the specific "educational activity" with pain specialists had been to foster clinical debate and understanding.
The company did not respond to BBC News's specific inquiries about the practice employed by some drug companies of monitoring the prescribing activity of individual doctors before and after hospitality visits.
The Association of the British Pharmaceutical Industry (ABPI) has since put further limits on the hospitality companies can offer doctors.
Dr Sheuli Porkess, executive director of research, medical and innovation at the ABPI, said: "In the UK we have strict rules around the marketing of medicines.
"If anyone has any concerns about the way that opioids are marketed, they should contact the Prescription Medicines Code of Practice Authority (PMCPA)."
Opioids can be effective for managing acute pain but long-term and high dose use can lead to addiction and increased risk of death.
Once a patient becomes dependent, withdrawal symptoms such as stomach cramps, diarrhoea or sweating, together with increased anxiety, can make it difficult to stop.
The "opioid epidemic" in the US is well documented. The numbers of deaths from opioid abuse have skyrocketed over the past 15 years, killing tens of thousands of Americans every year.
And pharmaceutical companies there are accused of using misleading claims and underplaying the risk of addiction to doctors and patients.
The dependence on opioids in the UK is nowhere near on the same scale as in the US.
But new research, external carried out at the Centre for Evidence-Based Medicine at the University of Oxford has found that the extent of the problem is far greater than previously thought.
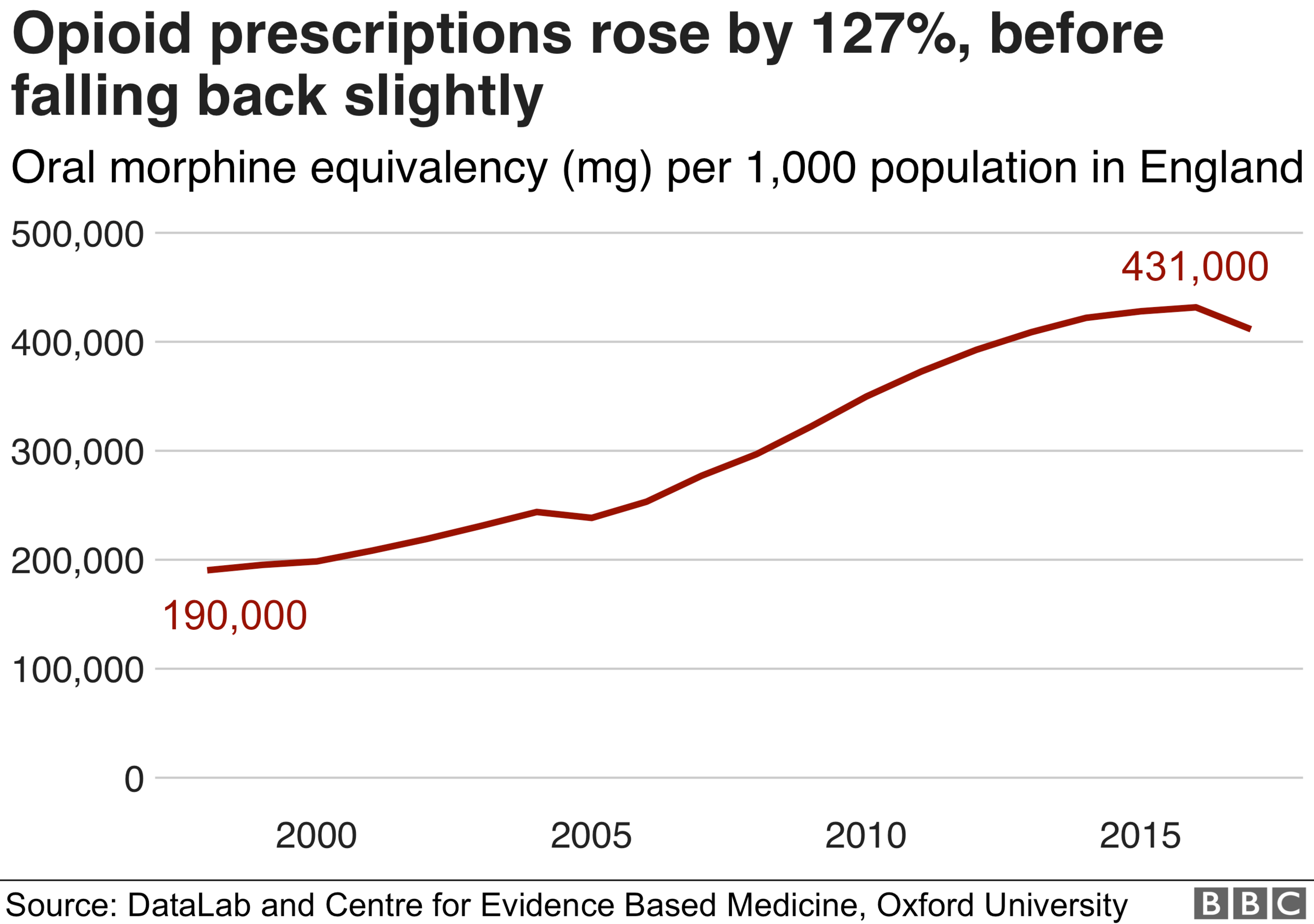
Researchers looked at trends and variation in opioid prescribing across England between 1998 and 2016.
'Spectacular increase'
When they counted the number of prescriptions, the increase was 34% - but when they accounted for the strength of the opioids prescribed, the increase was actually 127%.
The 34% increase took the number of prescriptions above 760 per 1,000 patients.
The 127% increase took the total oral morphine equivalency from 190,000mg to 431,000mg per 1,000 patients.
"Previous research had missed that spectacular increase because they didn't account for the fact that opioids that are being prescribed today, are much, much stronger," Dr Ben Goldacre told BBC News.
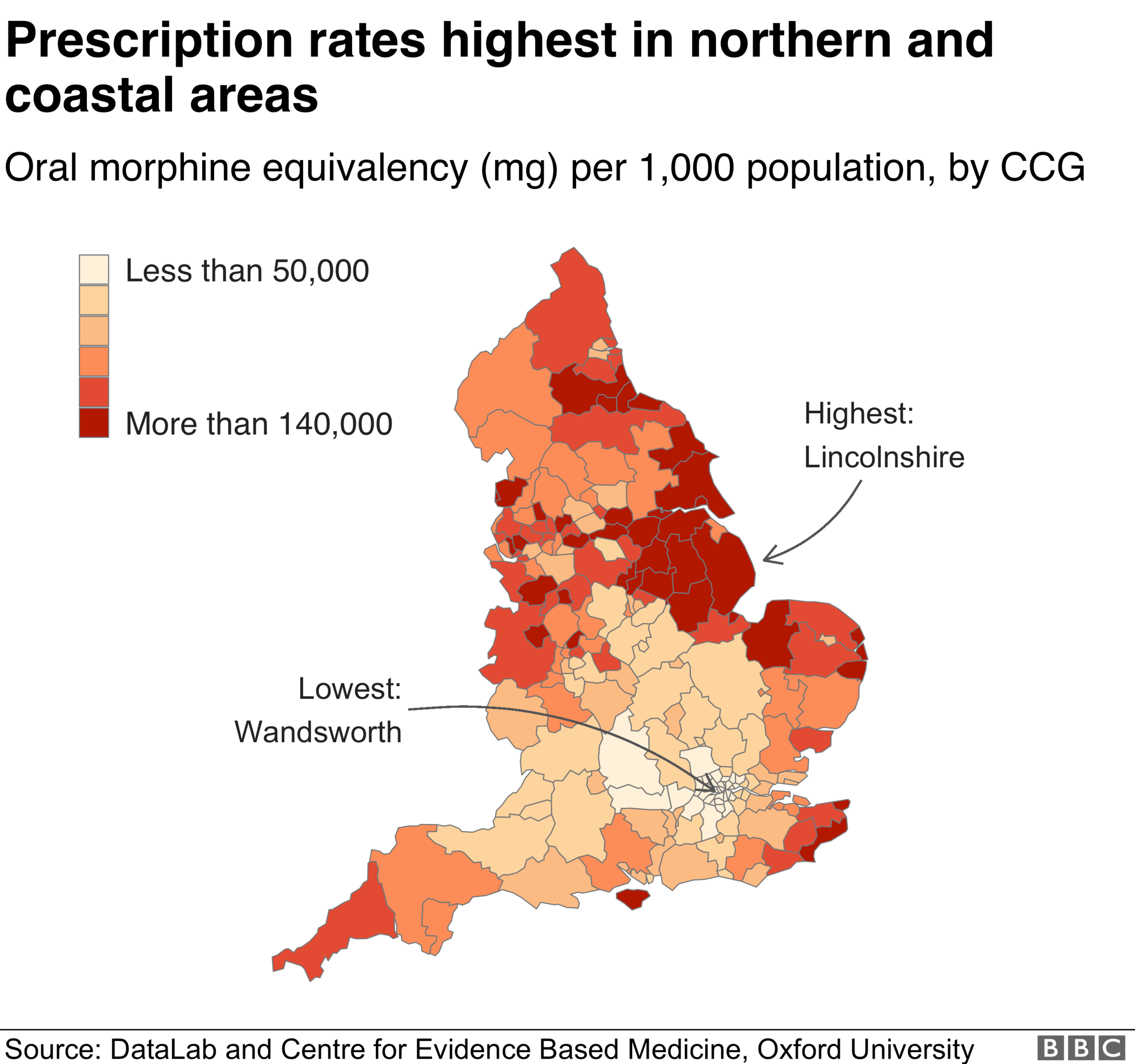
They also found GPs with more patients and in rural and deprived areas had greater high-dose prescribing rates.
Michael Richie, from Bradford-based drug treatment charity The Bridge Project, external, said: "Bradford can be gorgeous but it has its problems - deprivation, mainly, poverty, crime.
"I'm from a council estate myself but I see the more complex cases primarily from near areas with large housing estates in Bradford."
Sherry, who lives on a sprawling housing estate in the south-east of the city, has fibromyalgia, a chronic condition that causes pain all over the body.
Almost eight years ago, her GP began to prescribe her opioids - including morphine - for her pain.
Eventually, Sherry was taking the equivalent of 90mg of morphine a day.
She said the drugs had made it almost impossible for her to function - and she had still been in pain.

Sherry was prescribed opioids - including morphine - for about six years
"By the time I got up and dressed, it was time to get undressed," Sherry said.
"I couldn't do anything. The house was a mess. I was a mess. We were all a mess."
Around this time, Sherry's GP practice had become one of the highest prescribers of strong opioids in England.
It told BBC News it had since made considerable changes and reduced its opioid prescribing rates.
The Royal College of GPs told BBC News doctors were highly trained and prescribed in line with current guidelines - the lowest possible dose, for the shortest possible time.
In January, an expert working group of the UK's Commission on Human Medicines launched a review looking into the risks and benefits of opioid medicines.
Public Health England is currently reviewing the evidence for dependence on, and withdrawal from, prescribed medicines, and is expected to publish in the summer.
Opioid dependence is also a problem in Wales, Scotland and Northern Ireland.
Data journalism by Ed Lowther.
File on 4: Opioids: A Painful Prescription? is on BBC Sounds.
- Published5 February 2018

- Published22 July 2018

- Published28 April 2019

- Published24 February 2019

- Published28 April 2019
