Ex-health secretary pressed on reporting healthcare worker deathspublished at 15:06 GMT 21 November 2024
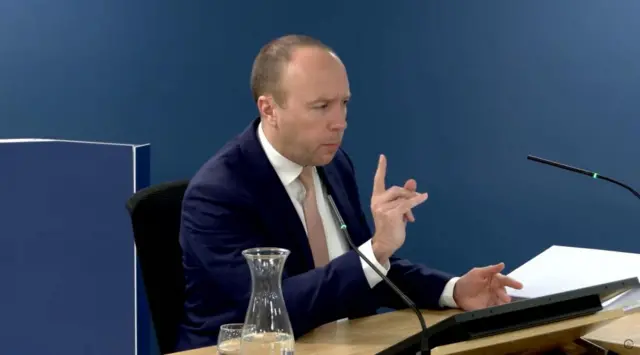
We're onto the final topic before a short break, with Matt Hancock being asked about systems for monitoring the deaths of health and care workers during the pandemic.
Hancock says there was no individual department ready to monitor this at first, but suggests that he went on to establish one.
Hancock is then pressed on whether he was aware of issues around under-reporting deaths of health workers and says he is "not surprised" before adding that statistical reports were largely wrong at the start of the pandemic.
There's then some discussion of statistical techniques that were used by Public Health England, and Hancock denies "quibbling" with them.
But, he stresses that the figures that were found were only a guide to the underlying truth of how many people were dying from Covid.
With that, the inquiry takes another short break.