Coronavirus: What can the 'plague village' of Eyam teach us?
- Published

The desperate urge to flee London risked spreading the plague across the country
With coronavirus putting households around the world in lockdown, can the English "plague village" of Eyam, which quarantined itself for more than a year, offer us lessons on how to fight back?
As a nightmare tale from history, Eyam's ordeal takes some surpassing.
When plague arrived in September 1665, rather than flee this wild corner of Derbyshire - and risk spreading the infection - villagers locked themselves away to suffer in isolation. And suffer they did.

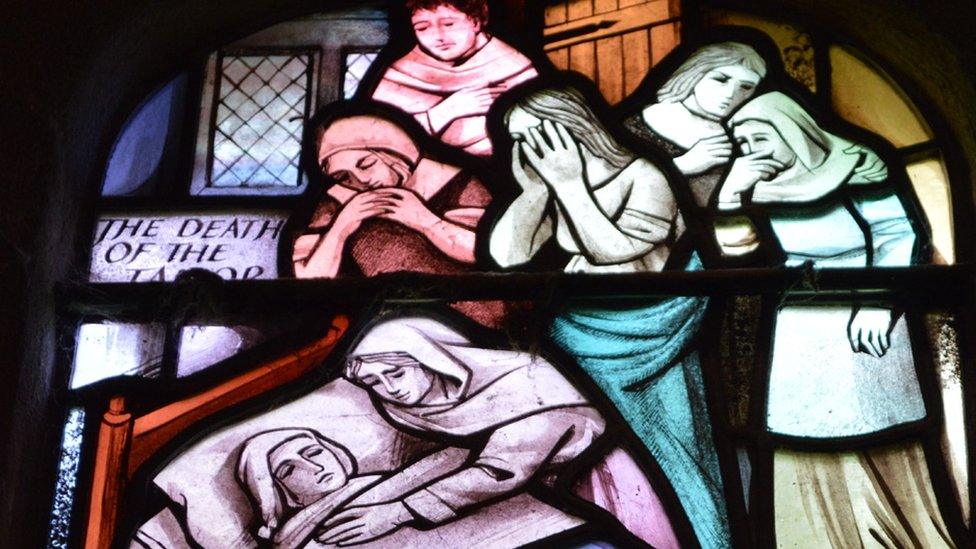
Eyam's story became well known during Victorian times as an example of self-sacrifice
For 14 months pestilence, pitiless and seemingly random, ravaged the village.
Deaths reached six a day, with one woman losing six children and a husband in just over a week. The graveyard was shut and bodies were dragged into fields for burial.
Traditional estimates put the death toll at about 260 - 75% of the population.
But along with gruesome tales of self-sacrifice, Eyam offers more - a unique opportunity to study how epidemics work.
And researchers have been trying to unlock its secrets to help fight disease - including coronavirus.

With the graveyard shut and funerals banned, the dead had to be dragged into fields for burial

Resident Joan Plant is related to one of Eyam's most celebrated survivors.
She said: "Margaret Blackwell was my nine-times great-aunt.
"According to family legend, while delirious with the plague she went looking for water to relieve her parched throat.
"By mistake she drank a jug of bacon fat. Soon after her fever broke and she made a full recovery."
The terror of the plague is evoked in this medieval image of death strangling a victim
All this begs lots of questions. Just how lethal was the disease? Why did so many die when families were isolated?
Did drinking bacon fat - or perhaps the instant vomiting this caused - really save Margaret Blackwell?
And perhaps most importantly, did the quarantine save others?
Can 21st Century science answer these questions and help us learn from the grim fate of one village 350 years ago?
The cause of plague - a bacterium called Yersinia pestis - was not discovered until 1894
It is a detective story of controversial ideas, new discoveries and hard lessons for today.
Sheena Cruickshank, professor in biomedical Sciences at the University of Manchester, said: "Learning about our history with disease informs our future.
"We know the immune system combines with other factors - the strength and dose of the pathogen, the health of the individuals, relative isolation - to determine the severity of the epidemic.
"Some factors - living in proximity to animals and affecting animal habitats - still play a role today with diseases like Zika, SARS, and coronavirus being shown to originate in animals "

With the arrival of coronavirus, isolation and quarantine have become part of everyday life for many
She added: "While many diagnostic details are missing, Eyam is a snapshot of how one community was shaped by - and itself shaped - the spread of a disease.
"And it is possible that survivors with more effective immunity led to part of the immune system of the survivors being selected for and handed down to following generations.
"As an example, some communities in Africa seem to have a higher incidence of a blood disorder - sickle cell anaemia - because it gave some protection against malaria.
"Reports have also shown that particular immune signatures were associated with more effective immune responses to plague and this can be tracked through generations."
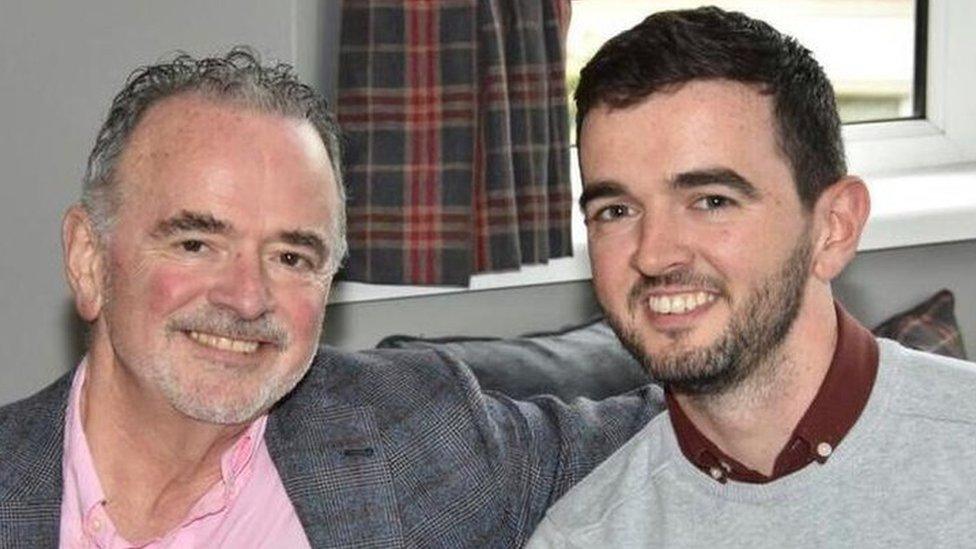
Fergal Keane met people in Eyam, the former 'plague village' in Derbyshire, dealing with coronavirus
In 2000, a team studying natural HIV resistance came to Eyam. They had a remarkable theory that built on the idea of inherited disease resistance.
A human gene mutation, called CCR5-Delta 32, was known to give immunity from HIV.
This mutation seemed to date from just a few hundred years ago and existed almost solely in north European populations and their descendants.
What could have caused it? An epidemic like the plague?
Team leader Dr Steve O'Brien later said: "Could it be that the same mutation that protects against HIV may have also protected medieval Europeans exposed to plague?
"The timing is right, the numbers are right - hundreds of years of unforgiving selective pressure from the sixth to the 18th Centuries would be sufficient to explain today's high CCR5-Δ32 frequency."

Plague: Forgotten, but not gone

Plague feels like a disease of the distant past but the cause, a bacterium called Yersinia pestis, was not identified until 1894 and it has never gone away.
In the late 20th and early 21st Century, 90% of reported cases of plague occurred in Africa, specifically eastern Africa, central Africa and Madagascar, with small outbreaks occurring in north Africa.
From 1958 to 2008, 17,000 cases were reported in Madagascar, 13,000 in Congo, 4,800 in India, and 438 in the United States. Hundreds have been reported since.
While the infection is treatable with antibiotics, bacteria are constantly evolving and in 1996 two drug-resistant strains of plague were isolated.
And while plague was first used as a biological weapon when diseased corpses were catapulted into the city of Caffa, in 1345, it didn't end there.
In World War Two the Japanese formed a bio-weapons unit which, among other things, spread plague-infected fleas over mainland China.
Both sides in the Cold War experimented with weaponised plague and while several treaties are now in place outlawing its use, Yersinia pestis is regarded as a Category A organism - a threat to national security - by the US.

Dr O'Brien tested 100 people who could trace their families back to the 17th Century.
It showed 14% of those tested had Delta 32, against a UK average of 10%.
Sceptics pointed out this higher percentage was not statistically significant and the pattern of Delta 32 went against the infection map of plague, which if anything hit southern Europe and Asia even harder.
Perhaps most significant, Delta 32 seems not to protect against plague bacterium, at least in mice.
But new revelations were around the corner.
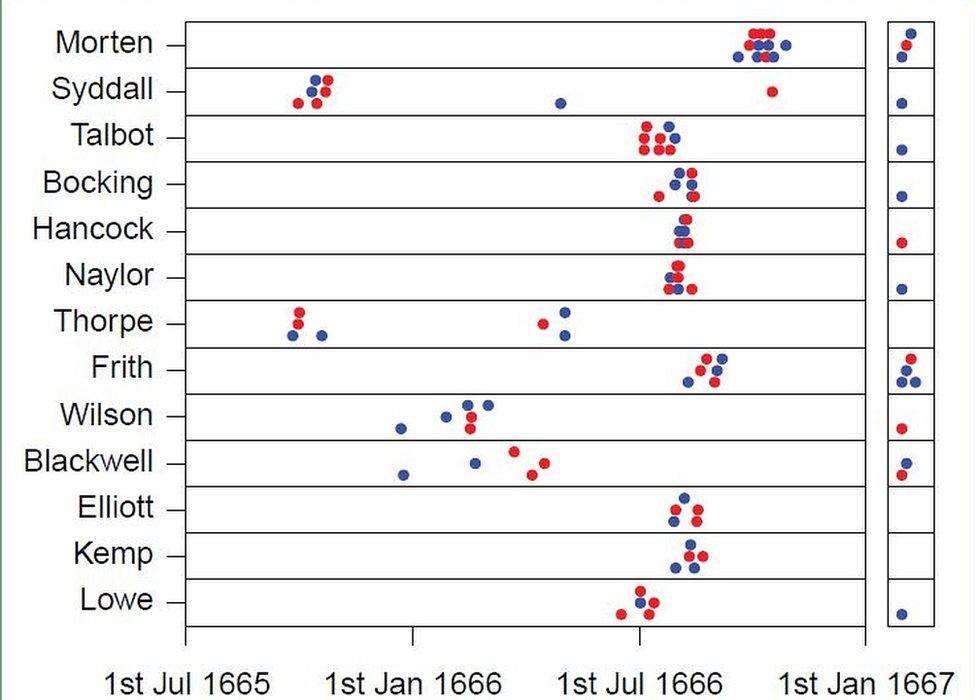
Graph showing how death hit families swiftly - blue for males, red for females, survivors on the right

In 2016 a study by Dr Xavier Didelot and Dr Lilith Whittles used analysis of local records to challenge some of what was understood about Eyam.
Significantly, it found the isolated population was at least 700, putting the mortality rate at a lower, but still horrific, 36%.

The village of the damned
When plague arrived in Eyam on a bundle of cloth from London, no-one could have foreseen the ordeal that lay ahead.
The following 14 months were characterised by death and disease, sacrifice and sorrow. The village's story has gone on to become part of English history as a symbol of selflessness.

Dr Whittles, infectious disease modeller at Imperial College London, said: "Eyam is important because it gives us fantastic data for the plague.
"We know about individuals, about households and particularly when people died. In larger populations, like in the cities, you only get weekly death tolls, which don't allow you to look at the finer patterns at the individual level.
"With the information from Eyam you can track how the disease is most likely to have spread.
"It has been understood, classically, that the plague spread from rat to human via the flea.
"We found human-to-human transmission during this outbreak - especially within families - was a much bigger factor than previously thought."

Studying how plague moved within Eyam, and particularly in families, offers lessons for the future
Dr Didelot said: "The risk of person-to-person transmission was almost two orders of magnitude larger if there was an infectious person in the household.
"Overall three-quarters of the cases were caused by person-to-person transmission.
"The main lesson here is that before imposing control measures to stop the spread of an infectious disease, it is essential to understand the way it spreads.
"There is often more than a single route of transmission, in which case it becomes important to estimate the relative importance of the various routes."
An additionally sad detail was the records also showed children and individuals living in poorer - untaxed - households were hit hardest, a factor still relevant today.
Another question this study answered was whether the village's isolation had helped stop the spread of the plague.

A SIMPLE GUIDE: How do I protect myself?
AVOIDING CONTACT: The rules on self-isolation and exercise
LOOK-UP TOOL: Check cases in your area
MAPS AND CHARTS: Visual guide to the outbreak

Some had suggested fleeing would have caused the plague-carrying rats to die off and the infection to burn itself out.
Dr Didelot said: "The importance of person-to-person infection showed isolation was the right thing to do.
"By staying within the confines of their community, the inhabitants of Eyam did indeed stem the spread of the epidemic, albeit at a tragic cost to themselves."
As for the case of Margaret Blackwell, Joan Plant thinks it is "very unlikely" that drinking bacon fat saved her.
"She was more likely lucky to have something in her genes - and perhaps that has been handed down through the generations.
"It is moving to think that the unimaginable sacrifice the villagers made benefited not just those communities nearby at the time, but is still benefiting the wider world now."

Follow BBC East Midlands on Facebook, external, Twitter, external, or Instagram, external. Send your story ideas to eastmidsnews@bbc.co.uk, external.
- Published3 April 2020
- Published22 February 2022

- Published7 May 2019

- Published5 November 2016

- Published8 September 2016
