Stroke patient died after surgery denial 'over lack of beds'
- Published

Nottingham University Hospitals NHS Trust would not accept Teresa Dennett for life-saving neurosurgery because its intensive care unit was full
A woman died after a hospital did not accept her for neurosurgery citing an intensive care bed shortage, an inquest heard.
Teresa Dennett, 58, needed surgery after a stroke and the coroner concluded "it is likely she would have survived" if the operation went ahead.
Nottingham University Hospitals said its intensive care unit was full and suggested she should go to Sheffield.
But NHS England said a lack of beds was not a reason for refusing admission.
Live updates and more from Nottinghamshire.
The death was highlighted by Heidi Connor, assistant coroner for Nottinghamshire, who has written what is known as a Regulation 28 report, external, which sets out aims to prevent future deaths.
She has sent the report to the chief executives of NHS England and two of the hospital trusts involved, following the inquest in Nottingham that ended on 6 January.
'Beds review needed'
She wrote: "In my opinion there is a risk that future deaths will occur unless action is taken.
"Crucially, it was clear there was no written protocol in place to set out a clear pathway for referral for emergency neurosurgery."
Meanwhile, the Royal College of Surgeons said it was "saddened" by the death and has called for NHS England to review bed capacity in the face of cuts.

What went wrong?

Teresa Dennett was admitted to King's Mill Hospital, which tried to arrange for her to have neurosurgery elsewhere
Mrs Dennett was admitted to King's Mill Hospital in Nottinghamshire on 6 February 2016 with a rare type of stroke
This hospital does not have neurosurgery services, so Mrs Dennett would normally have been transferred to the Queen's Medical Centre in Nottingham
However, Nottingham said all of its intensive care beds were full
King's Mill Hospital tried to arrange for Mrs Dennett to be treated in Sheffield instead - which is in a different catchment area
Sheffield said Mrs Dennett should go to Nottingham instead, as it was not aware there were no intensive care beds there
It was eventually agreed the patient should go to Nottingham and the bed situation would be resolved
By then Mrs Dennett had deteriorated too much for surgery to be carried out, and she died later on the morning of 7 February
The coroner wrote in her report: "Even if Sheffield had agreed to take the patient when first contacted, I found it unlikely she would have had the operation in time."

In response to the Regulation 28 report Prof Sir Bruce Keogh, NHS England's National Medical Director, has written to medical directors reminding them of national guidelines.
He referred to the Society of British Neurological Surgeons care quality statement (2015), which states: "The lack of critical care beds must not be a reason for refusing admission for patients requiring urgent surgery."
However in evidence, the inquest heard adopting the society's statement was voluntary, many of the neurosurgeons involved in the case had not heard of this statement before, and some described it as "aspirational".
NHS England must formally respond to the coroner by 30 June.

Responses from hospital trusts

The coroner sent her report to the chief executives of Nottingham University Hospitals NHS Trust (NUH) and Sheffield Teaching Hospitals NHS Foundation Trust (STH), which must respond by 31 March.
NUH said: "We extend our condolences to Mrs Dennett's family and apologise that we were unable to transfer her to our specialist unit immediately to consider surgery.
"We are working with partner hospitals to ensure more effective emergency care and transfers to specialist units in this diagnosis."
STH said: "If Nottingham had confirmed with us that they could not undertake the surgery, as per the clinical guidelines, we would have operated on Mrs Dennett in Sheffield regardless of bed availability.
"We will be discussing with Nottingham and King's Mill Hospitals the lessons which need to be learned in respect of the use of the clinical guidelines, so that the chances of this happening again are limited."
King's Mill Hospital is run by Sherwood Forest Hospitals NHS Foundation Trust, whose medical director Dr Andy Haynes said: "The coroner rightly praised our medical registrar for doing all he could to facilitate a very difficult situation."

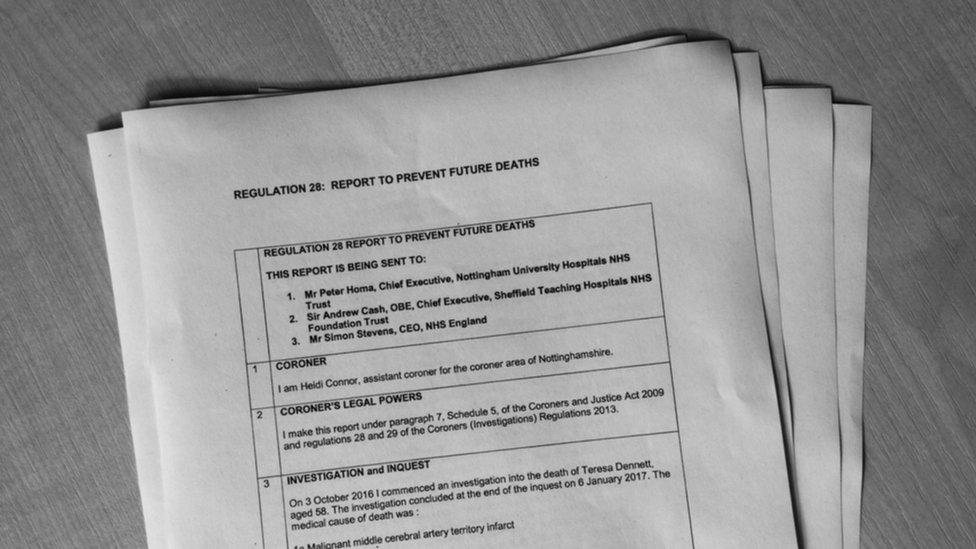
The coroner's report has been sent to the chief executives of NHS England and two of the hospital trusts involved
The inquest heard about a proposed new way of working whereby a patient who needs life-saving surgery would be transported immediately to their local unit.
This may mean a critical care bed would have to be found for the patient after the operation, even if that requires extensive "bed-juggling", as the coroner termed it.
In extreme cases, post-operative treatment could be provided elsewhere.
- Published15 February 2017

- Published20 January 2017
- Published13 January 2017

- Published12 January 2017

- Published16 December 2016

- Published7 December 2016
