'Life-saving drug' reverses 98 opioid overdoses
- Published

A medication that reverses an overdose from opioids, including heroin, has helped prevent deaths in 98 potentially fatal overdoses in the past five years.
Naloxone was introduced in Northern Ireland in 2012 and is funded by the Public Health Agency (PHA) and Health and Social Care Board (HSCB).
The PHA said the medication was used 112 times, and 98 were "successful".
"That's 98 incidents when someone could have died but didn't thanks to naloxone being administered," the agency said.
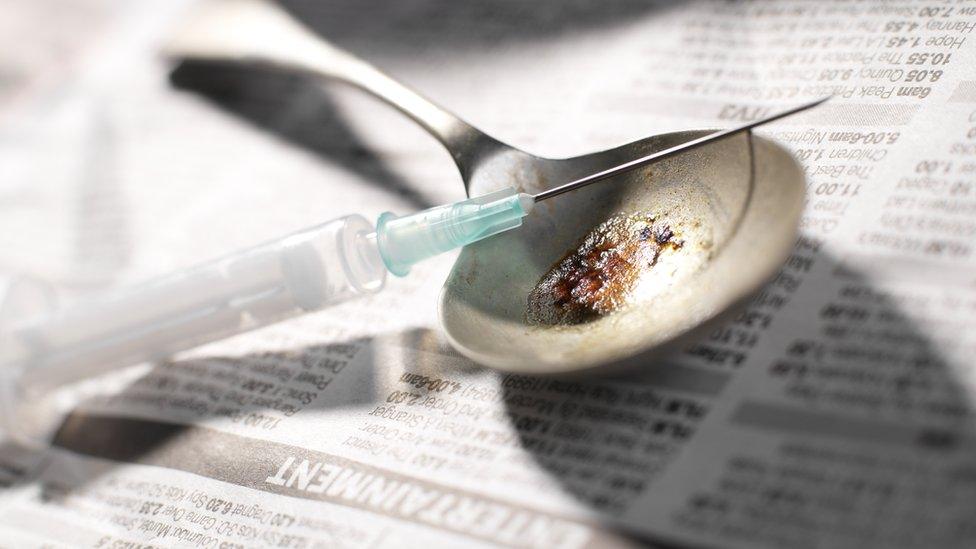
The main risks for people who use heroin or other opioids are transmission of blood-borne viruses through sharing of injecting equipment, and accidental overdose.
Naloxone temporarily reverses the effects of overdose, allowing more time for emergency treatment.
'High risk'
It can quickly restore normal respiration to a person whose breathing has slowed or stopped as a result of overdosing with heroin or prescription opioid pain medications.
The 'Take Home Naloxone' programme was introduced in July 2012, as part of the Department of Health's strategy to reduce the harm related to substance misuse.
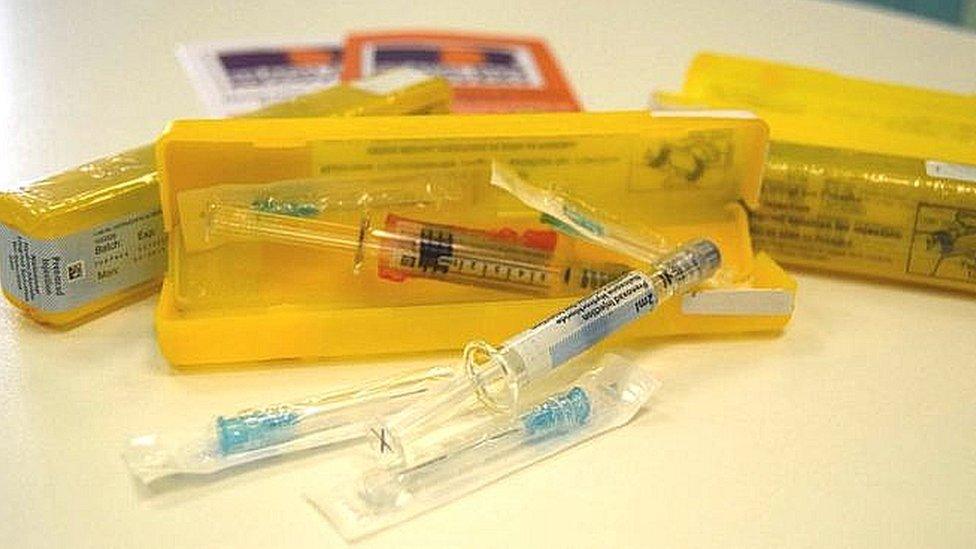
It comes in a pack containing syringes, and is supplied by the PHA to health trusts for distribution to homeless organisations, pharmacists, drug users and their carers.
Victoria Creasy, health and social wellbeing improvement senior officer at the PHA, said: "While only a very small portion of the population here use heroin or other opiate type drugs, those people who do are at a high risk of illness or death.
"It is therefore important that we look at ways that we can reduce the danger that these people face.
"Our priorities are to reduce these risks, through ensuring access to needle exchange services with trained staff, and providing access to naloxone.
'Successful'
"For the past five years, Take Home Naloxone has been available to anyone who is at risk of opiate overdose, through their local Trust Addiction Services or the Prison Service.
"By the end of March 2017, 1,250 packs had been supplied to those at risk."
She added: "The PHA is aware of 112 occasions when the Take Home Naloxone had been used to reverse an overdose, and of these 98 were successful; that's 98 incidents when someone could have died but didn't thanks to naloxone being administered.
"For each successful overdose reversal, £244 was spent on medicine."
The information the PHA receives on the cases where naloxone has been used to reverse an overdose is anonymous and is not linked with coroners reports, therefore the agency cannot comment on the causes of death in the 14 cases where nalaxone was used without success.
However, the PHA said factors which could increase the risk of death include mixing opiates with other substances, taking opiates which have been cut with other psychoactive substances, and using naloxone too late.
The PHA said they commission training which seeks to educate opiate users around these risks.
Iain Cameron works with the charity Extern and is one of the lead trainers for the naloxone program, he said the drug may actually have saved even more lives than reported.
"People may also use the drug and not report back that it has been used," he said.
"We believe it may have actually been used more than that."
Costs
Mr Cameron said it is "very easy" to teach people how to use the drug, "not only for people who might be addicted to opiates, but for anyone else who may come into contact with people who used opiates, to be taught in 20 minutes to half an hour how to administer this drug very safely".
The drug must be administered into muscle, normally the thigh, it has no effect on those who do not have opioids in their system.
Potential users must report that a pack has been used to get a replacement and they must complete training on how to administer the drug before it is issued to them.
The cost has increased slightly over the past four years, but on average, packs costs about £18.50 each.
This amounts to a total cost of £13,800 for the four years from April 2012 until end of March 2016.
- Published30 September 2016

- Published25 October 2016
- Published19 May 2011
- Published17 April 2017
