GP services: Extra £5.5m in GP funding for 'challenging winter'
- Published
- comments

The Department of Health is making up to £5.5m available to support GP services in Northern Ireland over winter.
Health Minister Robin Swann said he recognised the importance of people being able to access GP services.
The funding will be used to improve technology and accessibility, and support patient care.
Mr Swann said that services across health and social care were facing "a challenging winter".
He has allocated £3.8m to support additional patient care during this time and up to £1.7m to further improve telephone and computer technology.
He added that GP feedback showed that patients were presenting with more complex needs, making it difficult for GPs "to see all the people they would wish to".
Department of Health figures show that GP practices are currently carrying out almost 200,000 consultations on a weekly basis.
The health minister said that GP practices have been open throughout the pandemic and will continue to use both face-to-face appointments and alternative consultation options for patients.
He said work was taking place to improve access to primary care for patients, including exploring how telephone systems could be better used to support services.
He added that consideration was also being given to ways to better deal with routine requests, such as repeat prescriptions to release capacity.

Robin Swann says that primary care services in NI were "under increasing pressure" before the pandemic
"This work is part of a wider programme to help improve patient access to services, which includes the wider rollout of primary care multi-disciplinary teams, and work to reform the out-of-hours service.
"I am committed to ensuring that we have a GP workforce that is supported, motivated and sustainable and that continues to provide quality care to patients when they need it."
He said work was taking place on a review of GP trainee places, to make sure there were "enough GPs to meet our primary care needs into the future".
What are GPs saying?
Londonderry GP Dr Nicola Duffy said she had asked the Department of Health to be allowed to see more patients in person. She said they were currently restricted by policy.
She told BBC Radio Ulster 's Talkback programme that she was not allowed to see patients "without social distancing, wearing a mask, regardless of whether I am vaccinated or not".
"That is to protect the vulnerable patients that are using the health centre that I work in," she said.
"I am ready, my colleagues are ready. Could someone higher than me fix this, so we can get back to seeing our patients?"
Dr Alan Stout, chair of the British Medical Association of Northern Ireland, said he hoped the funding would help some of the immediate pressures that GPs were facing, "as well as beginning to address some of the more systemic and complex issues, including the number of GP trainee places available".
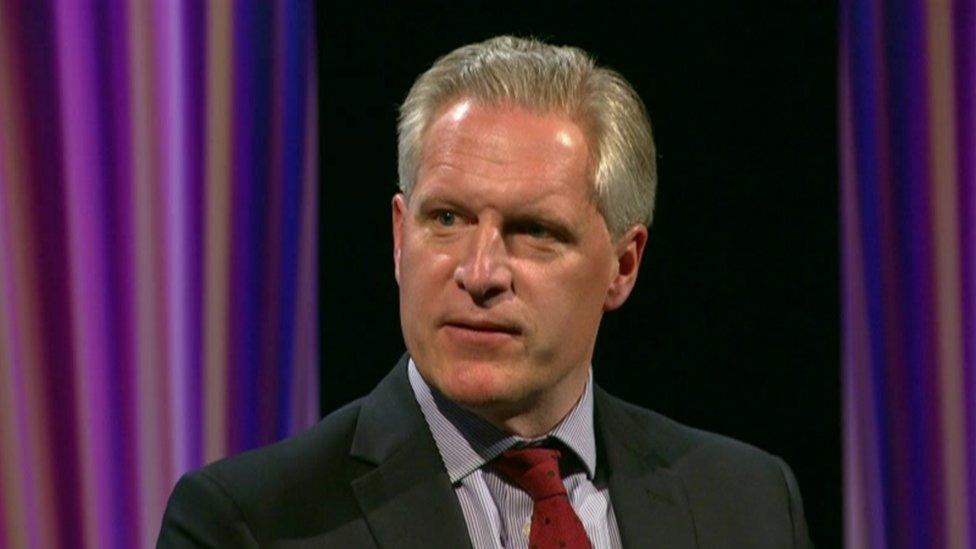
Dr Alan Stout from the BMA said general practice has "never closed"
"General practice has not closed and never closed," he said.
"Consultation rates and the number of patients contacting their surgery continue to be high and the current system is struggling to cope.
"All of our staff are feeling the pressure and we recognise that the difficulty in access and delays in seeing your GP cause frustration to patients."
But will the extra money help to resolve the current difficulties many patients are facing when trying to get a face-to-face GP appointment?
Dr Laurence Dorman, chair of the Royal College of General Practitioners Northern Ireland (RCGPNI), said the £5.5m was "very welcome" and would mean "extra surgeries and extra colleagues" to help meet patients' needs.
However, he said it was "short-term" funding and what was really needed is longer-term financial support and more GPs to join the workforce.
"At the moment, there's no point putting an extra phone line into our surgery if we don't have a GP at the end of those lines to meet the needs of our patients," he explained.
'Infection control'
Dr Dorman also warned that Covid-19 continues to pose safety concerns in GP waiting rooms, particularly for vulnerable patients who need to attend surgeries for treatment.
"We're still in the middle of a pandemic and we have to work the way we do to meet infection control standards," he told the BBC's Good Morning Ulster programme.
"We simply not like hairdressers and shops - we have sick patients coming into our buildings. We have patients who are taking blood tests, chemotherapy and we must be able to protect them," he said.
"We are seeing out patients face-to-face when it's appropriate and safe to do so, but we are still in a pandemic, we need our patients to work with us."
"But if our patients need seen face-to-face, absolutely then their family doctor will do that."

Dr Laurence Dorman said GP were still seeing patients face-to-face when it was "appropriate and safe to do so"
As well as his RCGPNI role, Dr Dorman works in a GP surgery in Kilkeel, County Down.
Addressing complaints over the number of in person appointments being made available, he argued that GPs were working "harder than ever".
Dr Dorman said the GP workforce was "tired and exhausted", adding that "some of the negative criticism is really demoralising".
'New ways of working'
He argued that the increase in telephone consultations during the pandemic meant that family doctors were treating more patients than they had ever done before and were often able to provide a "same-day" service.
He said GP services were undergoing an "overall transformation" like many parts of the health service, in an attempt to tailor services to patients' needs.
"This new way of working is actually suiting and working very well for some patients," he added.
Dr Dorman said that pre-Covid, most patients frequently faced a two-week wait for a GP appointment, most of which were face-to-face.
"That didn't suit a lot of patients, particularly patients who worked, patients who had caring commitments, so these new ways of working which are going right across the health care system, right through to outpatients and so on, are important and necessary."
- Published20 May 2021

- Published19 June 2020
