Infected Blood Inquiry: Delay in telling patients they had HIV
- Published
A group of Scottish haemophiliacs found to be infected with HIV from contaminated blood products were not told for two months.
The Infected Blood Inquiry was told 16 people were found to have the virus in October 1984 after receiving NHS blood products in Edinburgh.
But it was December that year before medics told patients that some of them might have been infected with HIV.
It was then left to them to ask whether they had tested positive or not.
The UK-wide inquiry is looking into what has been described as the worst treatment disaster in the history of the NHS.
Thousands of patients across the UK were infected with HIV - which can lead to Aids - and hepatitis C via contaminated blood products in the 1970s and 1980s.
The inquiry heard that by 1983, 10 haemophiliac patients in the United States had contracted Aids. The youngest was seven years old. Five of the patients died and the cases were linked to the use of a blood product, Factor VIII.
At that time, some Scottish patients were being treated with Factor VIII, produced locally by the NHS with blood donated in Scotland.
Prof Christopher Ludlam, a consultant haematologist and reference centre director at the Royal Infirmary of Edinburgh, told the inquiry that no cases of Aids had been reported in the Scottish population, so he thought the risk was "small but not zero".
Jenni Richards QC, counsel to the inquiry, asked: "There was no significant change of approach from 1983 to 1984 because you assumed that the concentrates you were using were safe?"
Prof Ludlum replied: "Yes, relatively or reasonably safe, I think that's fair, yes."
'Could have informed patients sooner'
In October 1984, without telling them, he sent samples from patients to be checked for HIV. Sixteen tested positive.
Prof Ludlum said the information was shared with a number of organisations, including the government.
The consultant said he was contacted by a reporter from the Yorkshire Post newspaper who wanted to run a story.
But he persuaded the reporter to delay publication and then invited patients to a meeting in Edinburgh Royal Infirmary on 19 December, 1984.
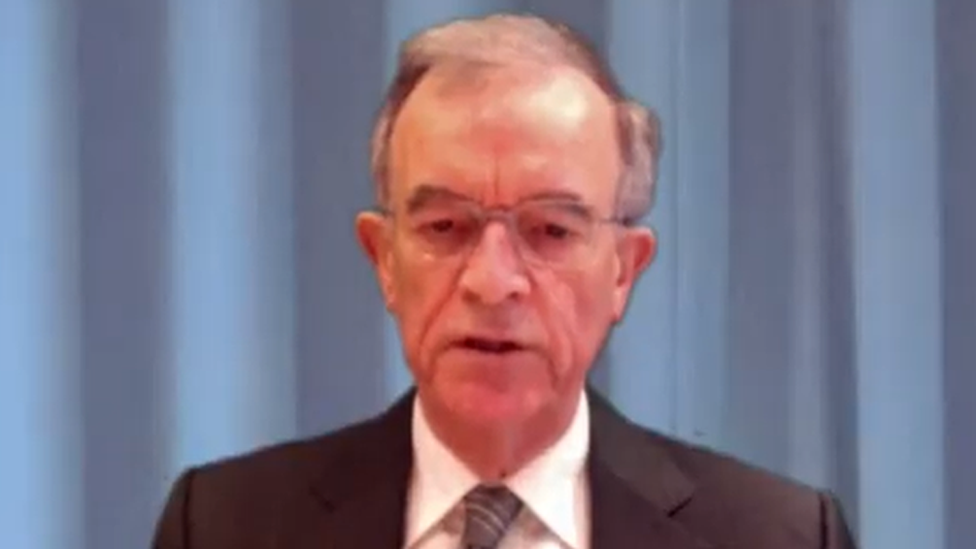
Prof Christopher Ludlam said it "took a bit of time for all the implications to sink in"
Prof Ludlum told the meeting about the test results and left it to the patients to decide whether they wanted further information.
Ms Richards said: "A number of organisations or individuals including ministers had been told of the situation. Patients at this stage are still in the dark. Why was it a difficult ethical decision to tell patients?"
Prof Ludlum replied: "We could have informed patients sooner but we were considering the best way to manage the situation and to think what we should be saying to patients and what patients would want to know.
"This took us very much by surprise and a lot of activity was going on and we needed to get our minds in order and decide what our systems should be. We didn't want information spread by rumour because that didn't help."
'Why the delay?'
Ms Richards: "You had known the result for 16 patients for nearly two months and had not told a single patient? Why the delay, Professor Ludlum?"
"The implications of it all were so enormous that it took a bit of time for it all to sink in and for us to think of the best way of responding," he said.
Ms Richards asked why it had taken so long to tell the patients when the risk from HIV transmission through sexual contact was known.
Prof Ludlum added: "It's easy looking back with literally 20/20 vision and although we knew there was a risk from sexual transmission, we had no idea how great the risk was, though we thought it was relatively small.
"It was a very difficult time and certainly I do see that in retrospect, maybe we should have done things differently and we certainly learned a huge amount from the way we responded to the whole of this."
The inquiry continues.
Related topics
- Published2 July 2019

