Contaminated blood scandal: Victims reveal 'coalition of secrecy'
- Published

Alistair Bennett's mother believes medics tried to "obscure" the cause of his death
A "coalition of secrecy" surrounded the contaminated blood scandal, victims have told an inquiry during the first of its sessions in Scotland.
One man told the hearing that medics knew he had Hepatitis C nine years before they told him.
And the mother of a man who died after contracting HIV/Aids from infected blood products claimed doctors tried to "obscure" the cause of his death.
The UK-wide public inquiry is in Scotland for two weeks.
It is hearing from patients who contracted HIV and hepatitis from contaminated blood products in the 1970s and 80s, and from the families of people who were infected.
Many of the NHS patients who were infected were haemophiliacs, while others included those who needed blood transfusions.
An earlier public inquiry into contaminated blood products in Scotland was labelled a "whitewash" by victims.
The Penrose Inquiry, external - published in 2015 - took six years and cost more than £12m, though its powers and terms of reference were limited.
What have victims told the inquiry?
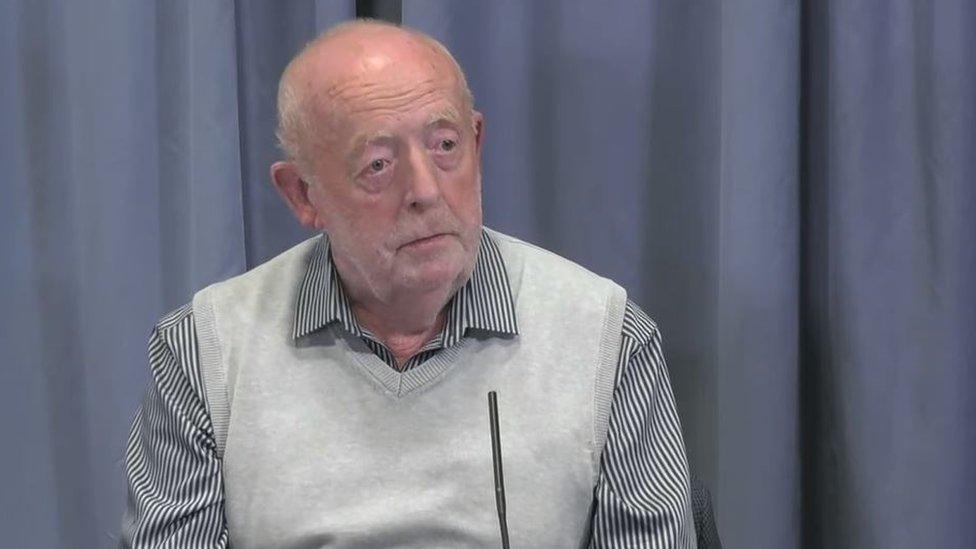
Thomas Griffiths had Hep C for nine years before he was informed
Thomas Griffiths, who was treated for haemophilia in Dumfries, said there was a "coalition of secrecy" around the scandal, and that more "honesty" could have led to better treatments and saved many lives.
He told the hearing he was reassured by his doctor and other medical staff when he raised concerns about the infections linked to blood clotting agent Factor VIII.
They told him they "never, ever" used imported blood products in Scottish hospitals - but he knew from the labels on the treatments that they came from Australia and the US.
It is now known that imported blood plasma came from prison inmates and drug users, who were at higher risk of blood-borne viruses like HIV and hepatitis.
The 75-year-old said he was eventually told he had Hepatitis C in 1999, but his medical records revealed his medics knew about the infection in 1990.
He said the doctor told him he had "nothing to worry about", adding that the doctor said: "The important thing about hepatitis C is that it's not life threatening, only life shortening."
Liver transplant
Mr Griffiths said: "When the horrors began to unfold there was widespread fear of how bad this might prove to be.
"This led to a coalition of secrecy I think, involving government departments, health service officials and indeed medical professionals.
"It should not take nine years to find out that you have tested positive for Hepatitis C and the condition progressed, of course, during all that time."
After a liver transplant in 2004, Mr Griffiths was free of haemophilia, and he was successfully treated for Hepatitis C.

Alison Bennett's son Alistair died after contracting HIV/ Aids
Alison Bennett's son, Alistair, died aged 22 after being infected with HIV while being treated for haemophilia in Manchester.
She believes doctors tried to "obscure" his cause of death by recording it as blood poisoning and bronchopneumonia with a secondary cause of haemophilia.
The main cause of his death was HIV/Aids, she said.
Both Ms Bennett, who now lives in Edinburgh, and her son Alistair were both diagnosed with Hepatitis C and she believes it came from a contaminated product.

Alistair Bennett was diagnosed with haemophilia when he was 10 months old
A third witness, who gave evidence anonymously, said he had attempted to take his own life after losing his partner and job having been diagnosed with hepatitis C, years after being given a blood transfusion following a lorry crash as a teenager.
Gill Fyffe, who received a transfusion of contaminated blood in 1988, will give evidence at the inquiry on Wednesday.
She told BBC Scotland she had "great hopes" for the new inquiry and described its chairman Sir Brian Langstaff as "extremely committed".
She said: "I think that because he's listening to evidence from so many victims, a true picture will be built of what people have suffered and what their losses have been.
"If you listen to those people who have already given evidence, it is absolutely heartbreaking."

Gill Fyffe had to give up her job after a blood transfusion 30 years ago
The latest public inquiry has been described as the biggest in UK history. It started in London in September last year and has already held sessions in Leeds and Belfast.
It aims to establish why patients were given blood products infected with HIV and hepatitis C, and whether there was a cover-up.
The Department of Health estimates that 30,000 people across the UK were affected.
The inquiry, before former High Court judge Sir Brian Langstaff at the Edinburgh International Conference Centre, continues.

Analysis
By Lisa Summers, BBC Scotland Health and Social Care Correspondent

In contrast to the rest of the UK, Scotland was less reliant on imported blood products from the US.
The transfusion service, however, regularly used donations from prisoners to top up supplies - a group at higher risk of having infections like HIV or hepatitis C.
So for the Scottish patients, who felt that they had no voice in the Penrose Inquiry, this is an opportunity to discover where responsibility lies for those actions.
But this new UK wide inquiry is also broader and has greater powers. It will look at claims of a cover-up, and the response of government and officials as the risks began to emerge.
And like thousands of others across the UK, the key questions are similar: will it hold people to account? And will it result in more compensation for the victims and families who have lived with the stigma, or died with the shame, of this enormous NHS mistake?
- Published24 September 2018
- Published20 June 2019

