Analysis: GP shortages 'crisis' and rural NHS in Wales
- Published
The health minister said the number of GPs in Wales has moved through the 2,000 barrier for the first time this year, while patient satisfaction is "eye-wateringly high".
But the Royal College of General Practitioners (RCGP) in Wales has pointed to a "desperate workplace crisis" with too many GPs leaving on the one hand and a slump in the young medical graduates looking to train as GPs.
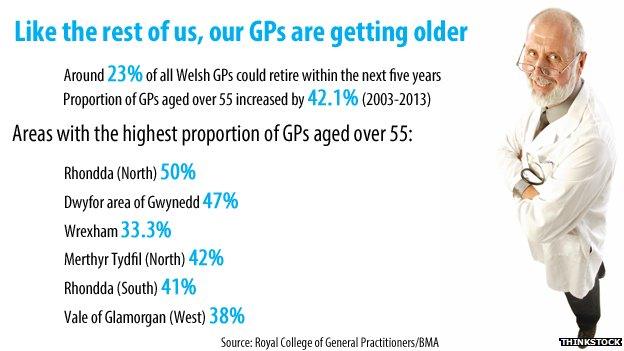
OLDER GPS LEAVING
There have been suggestions of "golden handcuffs" incentives to stay on.
But doctors' leaders have also pointed to the bureaucracy for GPs who may wish to work part-time after retiring - or continue to practice occasionally at peak times. The assembly's cross-party health committee has taken this on board and is recommending ministers encourage more to stay on and work flexibly.
The RCGP in Wales though has no doubt as to the main reason.
"We are seeing people leave at the age of 58, 59, 60 whereas, previously, GPs would go to 65 or 70," according to chairman Dr Paul Myers.
"I know there are issues about pensions and 40% taxation and everything, but I think the real issue is about workload. We're worn out."
He added: "Such is the shortfall in the number of family doctors that general practice is simply unable to keep pace with the growing patient demand generated by a growing and aging population."

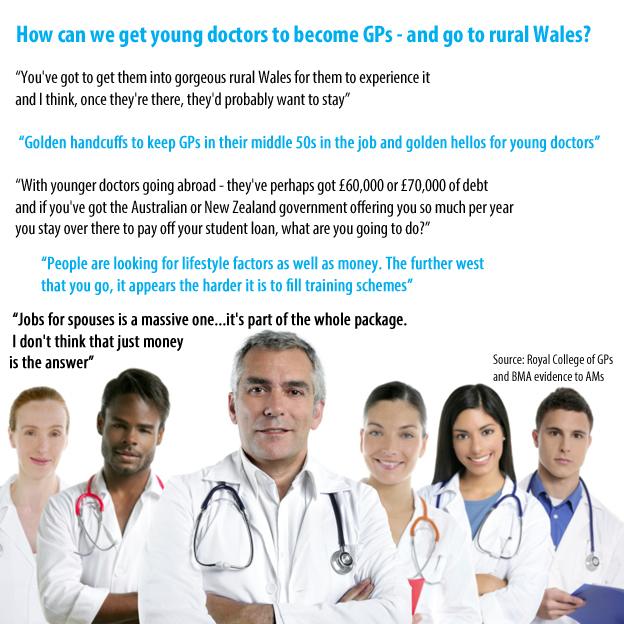
FEWER YOUNG DOCTORS TRAINING AS GPs
There is a target of 136 specialist GP trainees in Wales - set a decade ago - but the British Medical Association would like to see 200; and an extra 50 trainees to match England.
It said it is "quite staggering" that Wales has the lowest number of young doctors in GP practice as part of their second foundation year - just 24% compared to a 55% average across the UK. In the north west of England, 95% of students get a taste of working as a GP.
GP trainees tend to get paid less than hospital trainees, which are higher banded as the work is more highly intense. There was also thought to be some negative attitudes towards working as family doctors compared to jobs in hospitals.
The assembly health committee looked at GP recruitment recently and made a number of recommendations, including:
Offering incentives aimed at keeping GPs in parts of Wales where it has been harder to recruit them, such as rural areas and ones with high deprivation
Trainee doctors should get the chance to find out what it's like to be a GP before they decide on their specialty.

CHALLENGES AND POOR MORALE IN RURAL AREAS

Patients feared a downgrading of Bronglais Hospital
Health economist Prof Marcus Longley recently looked at the challenges to hospital and GP services in mid Wales and compiled a 200-page report.
He found that Bronglais Hospital in Aberystwyth - the only general hospital in mid Wales - had been "dogged by uncertainty" but delivered services well.
But it needed to make "significant changes" in ways of working, while recruitment was an issue.
Patients voiced a huge amount of support for Bronglais, while facing "draining" amounts of travel for specialist appointments at other hospitals.
Other issues which could help meet rural challenges, highlighted by Prof Longley:
More integrated health and social care, such as the £5m centre in Builth Wells and another planned in Tregaron.
Looking at the development of the concept of a "rural GP", expanding salaried GPs, and a fresh look at how to generate additional paid opportunities for GPs.
Developing GP clusters - GPs working together covering populations of 50,000, pooling resources and sharing specialist nursing and other services like pharmacies, dentistry and therapies. There are already 64 clusters. The Welsh government wants these to be at the forefront of tackling the most disadvantaged and most at risk of poor health and wants action plans to develop them.
Meanwhile, Prof Longley said he was struck by the "generally poor morale" amongst many GPs who felt the service changes were not enough to meet the scale of the challenges they faced.
Future technological advances - e-consultations, remote monitoring, tele-radiology and even e-ICUs (intensive care units) will offer new opportunities
Meanwhile the Welsh government has unveiled a new contract to allow GPs to spend more time with patients.
It is also about to launch its own report into GP workforce issues, alongside its three-year plan for services.
"Innovative clinical solutions, designed in collaboration with local populations, will help to make mid Wales a centre for rural healthcare excellence," said Health Minister Mark Drakeford.
- Published12 March 2015

- Published2 March 2015

- Published12 March 2015

- Published20 February 2015

- Published20 February 2015

- Published24 January 2015

- Published24 October 2014