Q&A: Is Wales' patients' watchdog showing its teeth?
- Published

Peter Meredith-Smith joined the CHC board last July
Community health councils (CHCs) in Wales are to re-launch themselves at their annual conference after admitting many patients do not know they exist.
The watchdogs, which have been going for 40 years, want higher profiles as bodies which can raise concerns about the NHS when things go wrong.
They admit public awareness is "poor" and a "real weakness".
It is set against a background of controversy about hospital reorganisations, A&E waiting times, ambulance response times.
We asked Peter Meredith-Smith, director of the Wales board of Community Health Councils,(CHCs) about the challenges facing the network of eight watchdogs across Wales.
He is a former nurse and an ex-official with the Royal College of Nursing and has also been a senior official involved in nursing and mental health with the Welsh government.

Community Health Councils in Wales include local councillors and appointed members
Is the biggest problem facing CHCs that patients do not know who you are and how to make a complaint?
The public that engage with the CHCs very much value the role that we play in overseeing their NHS and are appreciative of the support they receive when they need help in raising concerns.
However, it is disappointing that we have been described as "the best kept secret in Wales". One of our highest priorities going forward is to increase public awareness of CHCs.
As the statutory NHS Wales watchdog we represent public and patient interests in healthcare, so it is important that they know we exist and how we can help them.
Lack of public awareness of the CHCs' independent advocacy service was a finding within Keith Evans's review of NHS complaints handling last year; we are addressing that now.

Is this about persuading the public that CHCs are independent bodies which work in their interest, rather than in the interest of health boards or the government - has this been a problem in the past?
As statutory, independent bodies representing the interests of the public and patient in health, the CHCs always put the interests of the public we serve at the heart of our work.
Our regulations, which have just been reviewed, underpin our role and our independence from the NHS that we scrutinise. Notwithstanding this, it is essential that we enjoy a trusting and constructive relationship with the NHS organisations across Wales that we oversee.
We work closely with them to ensure services are safe and represent the patient interest in any service changes proposed.

What three issues have you as a group been seeing over the past 12-18 months which keep coming up?

Pressures on hospital A&E is still the biggest concern among patients
The first is probably the major concern relating to the pressures on accident and emergency departments across Wales and the UK as a whole. This is a serious systemic issue, resulting in ambulances being unable to discharge patients in a timely way.
The second, relating to this, is the generally high level of delayed transfers of care, where hospital beds are needlessly occupied because of problems discharging them to community-based care.
The third relates to the delays in actually realising "integrated healthcare". There are some good examples of best practice, but the bridge between health and social care is still a very narrow one.

If I had a concern about the care of a relative in a nursing home - or even in his or her own home - how would you like to see it work in future?

Worries about elderly people being malnourished and alienated in some care homes have been raised by the older people's commissioner
The CHCs have a right to inspect the NHS care received by a resident in any care home setting.
As part of our programme of collaboration with other inspectorates, we are currently working closely with the Older People's Commissioner in Wales and will also be approaching Care and Social Services Inspectorate Wales, (CCSIW) to see how we can deliver more comprehensive healthcare scrutiny for residents in nursing home environments.
NHS care is just one aspect of this; we need to ensure that the care home environment as a whole preserves the dignity and overall well-being of the resident.

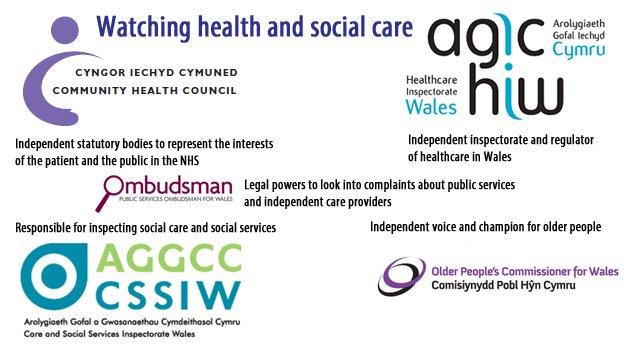
Several organisations cover health and social care in Wales
You are looking to work more closely with bodies like Healthcare Inspectorate Wales and the Older People's Commissioner. Is how the NHS is monitored too bureaucratic?
We have learned much from the Francis Inquiry into the Mid Staffs Foundation Trust, which said that when public bodies responsible for protecting the interests of patients fail to collaborate "the consequences can be disastrous".
It is quite clear that CHCs must work closely with bodies such as HIW, CSSIW and the Older Peoples' Commissioner.
CHCs represent the public and patient - it is vital that intelligence derived from this vital source is aggregated and fused with intelligence from other sources.
Given the size and increasing complexity of the NHS, as well as the changing demographic healthcare needs, we must pool intelligence in order to identify the crisis points quickly and do something about them.

What can you practically do about an issue like ambulance waiting times, for instance?
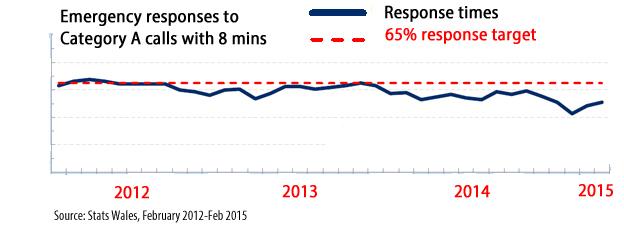
Ambulance response times against target for the last three years
The issue of pressures on ambulance service across Wales is a very serious one. It features high on the list of issues of concern raised with us by the public.
It is also regularly at the top of agenda during our regular engagement meetings with health board directors.
This issue is symptomatic of systemic problems with the health and social services in Wales. We are working hard locally and nationally to ensure that health service planners and providers improve things.
We are working with the Welsh Ambulance Service on very practical day-to-day issues and are part of the Welsh government project that is looking at developing whole systems solutions to very real challenges relating to unscheduled care that we are experiencing in Wales.

Patients have been very vocal about protecting local hospital services, especially in more rural areas. Are they really being listened to?

Campaigners have protested about hospital services in Haverfordwest being 'downgraded'
A vital CHC function is public-patient engagement. It is a two-way process; we listen to the public and convey those concerns to the NHS service provider.
In turn, we must understand why services need to change and pass that understanding to patients.
Accessing services in rural areas is a key area, where distance and transport issues can be exceptionally worrying. For example, maternity services, stroke services and care of the frail and elderly, where time is of the essence.
We work hard to ensure that these concerns are included in LHB [local health board] planning processes. Safety is key - 'safe services as locally as possible', as opposed to, 'local services as safely as possible' is a major factor.
All too often the public feel that they have not been listened too, eroding the trust and confidence they have in the LHB.

Can you strike a balance though - do you also need to make the case for change, which is advocated by professional bodies like the royal colleges, for example?
What clinicians say regarding the safety and effectiveness of services is vital and we always give careful consideration to what they have to say. The CHCs are responsible for representing the crucial "lay interest" in health service issues and what "real effect" the changes have on local populations.
It is becoming more and more the case that certain healthcare services are centralised in fewer centres of excellence, often meaning that the patient has to travel further to access it, but the care and outcome is considerably improved.
We work hard to ensure that any decisions made properly factor in the public and patient opinion, and that LHBs, in particular, pay this due regard and allow time to factor this in.

Can you identify weaknesses in the way CHCs have been operating up until now. How can the system become more effective in future - what have you achieved since the Longley review?
Since the Longley Review of CHCs was published in 2012, our board has been working hard to address the recommendations made in this important report.
The most recent Welsh government consultation on our regulations has taken account of these. In future the seven CHCs across Wales will be working to consistent standards, but at the same time maintaining our local "reach", sensitive to local differences. The CHC board will monitor these standards.
We have already reviewed our advocacy service and work is in hand to introduce common standards to this important service, as well as our inspection and engagement functions.
We will also be developing our relationships with other bodies like HIW, CSSIW and the Older People's Commissioner - that has been a weakness in the past. We have now produced a statement of strategic intent, which will focus our functional development over the period 2015-2018.

How exactly will you strengthen collaboration with other health bodies like the Health Inspectorate Wales?
We have already developed a protocol with HIW which allows for regular and routine exchange of information and intelligence and the potential for joint inspections. In 2014, we carried out a number of GP inspections across Wales together and we will look to mount more of these. This will be formally exchanged at our annual conference in Cardiff.
Work is also ongoing with the Older People's Commissioner to examine how we can more effectively represent the interests of care home residents.


Lilian Williams, 82, was seriously neglected at hospitals in Neath Port Talbot and Bridgend before she died, prompting a review by Prof June Andrews
Does Prof June Andrews's report and other examples of concerns about standards of care demonstrate weaknesses?
Unfortunately they do. The NHS is a human service and occasionally things go wrong. When they do, we need to acknowledge and recognise them and ensure that they form part of the learning process to prevent them happening again.
Many of the recent reviews, like the Andrews' Report, external and the Evans' Review comment that health boards must have intimate contact with what is happening on their frontline - the wards for instance. The CHC work closely with LHBs to ensure that any shortfalls are dealt with quickly and effectively.

How do you get the public to engage more with your work. Are you user-friendly enough?
One of our primary objectives going forward is to further develop our public patient engagement strategy. This is a vital function - we cannot act as the patient's voice unless we reach out to them, right at the local level - and they can reach us with their comments and experiences.

Do CHCs in general need to be more outspoken? Notably North Wales CHC has been particularly public in its criticism of recent decisions on changing obstetric services by Betsi Cadwaladr Health Board?

1,500 people protested about maternity service changes at Glan Clwyd Hospital, Denbighshire, last month
The public need to have confidence that we will represent their healthcare interests at every opportunity in an honest, transparent, and visible way. We work closely with LHBs and they are legally obliged to keep us informed of any service changes right from the start.
We also have the statutory right to refer any concerns that we cannot resolve locally direct to the health minister. In north Wales, the CHC acted on public concerns relating to obstetric services and brought those concerns to the attention of the health minister.
- Published26 March 2015

- Published13 May 2014

- Published2 July 2014

- Published22 February 2015

- Published16 October 2014
