Antibiotic resistance: Welsh public panel listens to experts
- Published
A "citizens jury" has been looking at the part Wales can play in tackling the global threat of antibiotic resistance.
For the last 70 years there has been a reliance on drugs to fight common infections but bacteria has been mutating to fight back.
The issue of resistance to antibiotics has been compared to climate change or global terrorism.
A panel of 14 people have been listening to experts in Cardiff in what has been called a "world first".
It is understood this is the first time members of the public have been brought together in this way to discuss what has been called the world's "ticking time bomb".
Behind it is the fear that the drugs and medicines depended on to kill bacteria could one day become obsolete.
Beth Clarke, 34, has had cystic fibrosis since she was a baby and needs to take antibiotics to live.
This could mean what is considered to be routine surgery today could become deadly in 20 years time.
The problem is that bugs that can cause harm are becoming more and more resistant to antibiotics - which has led to the emergence of so called "superbugs".
But why? One problem is that the more often antibiotics are used the more quickly bacteria build up resistance.
Another issue is that no significant breakthrough has been made in the discovery of new types of antibiotics for almost three decades.
One expert said drugs companies found it more profitable to be developing other medicines.
So what should be done? Are patients demanding too many antibiotics for minor illnesses - are doctors too willing to hand them out? Why is not more being spent on research into developing new antibiotics?
The members of the public will be listening to the experts - but also giving their own views.
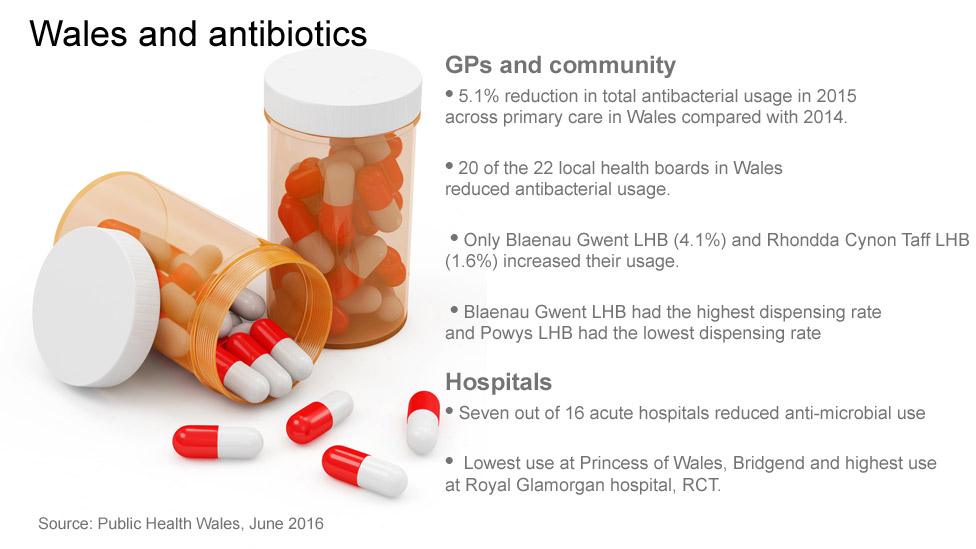
As it stands in Wales, there is good and bad news.
There has been a drop in prescribing antibiotics in seven of Wales' 16 acute hospitals and a 5.1% fall in prescribing by GPs but there is still room for improvement.
Dr Robin Howe, lead for anti-microbial resistance at Public Health Wales, said the aim was to stop over-use of antibiotics by GPs and in hospitals.
"In Wales, there are just over 3 million prescriptions every year and about a third of those are probably unnecessary," said Dr Howe.
"In hospital, there are the same sort of numbers of antibiotics - for every patient in a hospital bed in Wales every day, there is a dose of antibiotics given; again these are unnecessary levels."
Terence Canning, Welsh director of the Sepsis Trust, tells the story of his brother Mark (left) who died of sepsis
Dr Howe said resistance was increasing so patients were recovering more slowly, there were more complications and increased bloodstream infections like sepsis which were leading to deaths.
"If you get sepsis you have a one-in-five chance of not coming out the other end," he said.
Although there were no untreatable bugs in Wales yet, they exist in south east Asia and China and they could arrive here because of tourism.
Prof Jonathan Richards, former Merthyr Tydfil GP and clinical adviser to Cwm Taf Health Board and Public Health Wales, said while there had been changes in how antibiotics are prescribed and used, it was like turning an oil tanker around.
"A lot of doctors think what patients want is a prescription so the easiest way to get them out of the door is to give them what you think they want," he said.
"What we know now is that a lot of people are much more sophisticated and they want an assessment and the doctor to give a judgement as to whether antibiotics might help."

VIEWS FROM THE PANEL
One of the panel Beth Ward gives her impressions before - and on the last day
Beth Ward, Ruthin, Denbighshire; product designer.
Thoughts before: "I feel like it has the potential to be a huge problem. I've come in pretty blind but I'm looking forward to learning. I don't know enough about the science behind it. It's our opportunity to have our say and there are people from different backgrounds and a huge demographic."
Thoughts on the final day: "What's been a recurring theme is a lack of education and information for the public. There's a lot of information out there but none of us had any idea about it. It needs a very big behavioural change."
Eurig Lloyd, Porthcawl, Bridgend; former head teacher.
"I want to know how we can help the situation - and the situation is grave. If we don't do anything about it many of the diseases we're able to cure today - like TB - we won't be able to cure. We're all responsible, the public and the NHS."
Emma Smart, Cardiff; project manager.
"What's really struck me most is the scale of the problem. There's definitely not an overnight solution. It's going to need a lot of people working together and some sort of centralised taskforce is what I'd put forward."
You can follow proceedings on Twitter: @antibioticjury


The panel has been meeting all week in Cardiff
Dr Chris Jones, acting chief medical officer for Wales, said if no action was taken then there was a risk the medicines depended on to kill bacteria could become useless.
He said it was as much an issue for the public as for the NHS.
"The public expects antibiotics, often when sometimes they're not necessary," he said.
"We need to raise awareness of why not everyone will get an antibiotic when they feel like they should get one."
Dr Jones added: "The danger is we won't have effective antibiotics for serious infections - procedures, operations, surgery, chemotherapy for cancer where your immune response is reduced.
"Those situations, where we think we routinely have antibiotics available, may become more dangerous."
The idea behind the panel is for professional bodies and experts to be challenged by some "healthy realism" from the public.
Later in the process, panellists will be given reports on how their views have been taken on board.
Dr Jones said: "I want this group not to be a talking shop but I want its advice to be heeded so it makes a difference."
- Published8 July 2016

- Published6 May 2016
- Published10 October 2014
- Published19 November 2015

- Published11 March 2013

- Published3 July 2014

- Published19 November 2015
- Published8 July 2016

- Published8 July 2016
