Ambulance response times: Only Wales sees improvement
- Published
- comments
Take our animated road-trip of ambulance issues in Wales
Wales is the only UK nation to see an improvement in the time it takes ambulances to reach the most critical 999 calls, new BBC research has found.
The health secretary said it shows a "better service with a better outcome for patients".
It follows controversial changes in the way 999 calls are prioritised.
But like other UK colleagues, Welsh ambulance crews are facing worsening delays in handing over patients when they get to hospital.
The statistics from the BBC's freedom of information request revealed that average response times for calls, where a life is judged to be immediately at risk, have improved since a new "clinical model" came into force in October last year.
In contrast, the trend in England, Scotland and Northern Ireland appears to be in the opposite direction.
The changes in Wales saw response-time targets scrapped for all except the most serious cases.
Before then, an eight minute target applied to about 40% of calls received by the Welsh Ambulance Service.
Now the eight minute target applies to just 4 to 5% of the calls received designated red under the new system.
Opposition parties at the time criticised the change as "moving the goal-posts" and the Conservatives believe the current categorisation is still too narrow for the most urgent cases.
But Health Secretary Vaughan Gething said: "It's meant we're going after people where that fast response makes a difference.
"And that was the whole point for the change - it's not because it's easier for a politician to do but because there's evidence and advice from leading clinicians that this is the right thing to do for patients."
The latest performance figures, out on Wednesday, show 77.1% of responses to red calls arrived within eight minutes, external. The target is 65%.

BUT HANDOVER DELAYS ARE INCREASING
Despite improvements in response times, the figures showed that ambulance crews face worsening delays outside A&E departments.
These are caused when emergency units become full, meaning patients have to wait in an ambulance for beds to become available.
When this happens the ambulance and crew cannot respond to other calls.
The figures for 2016 are worse for every month compared to the same month last year - despite commitments by health boards to try to tackle the problem.
The worst period was in March at the peak of the winter pressures.
In total, ambulances have spent more than 40,500 unnecessary hours waiting outside A&E between January and August - nearly as much as for the whole of 2015 already.
Sonia Thompson, head of operations for the Welsh Ambulance Service in north Wales, said it was a complicated issue and they were working closely with hospitals and health boards to tackle handover issues.
"We need to understand demand and ensure if someone doesn't need to go to hospital there are alternatives to use," she added.
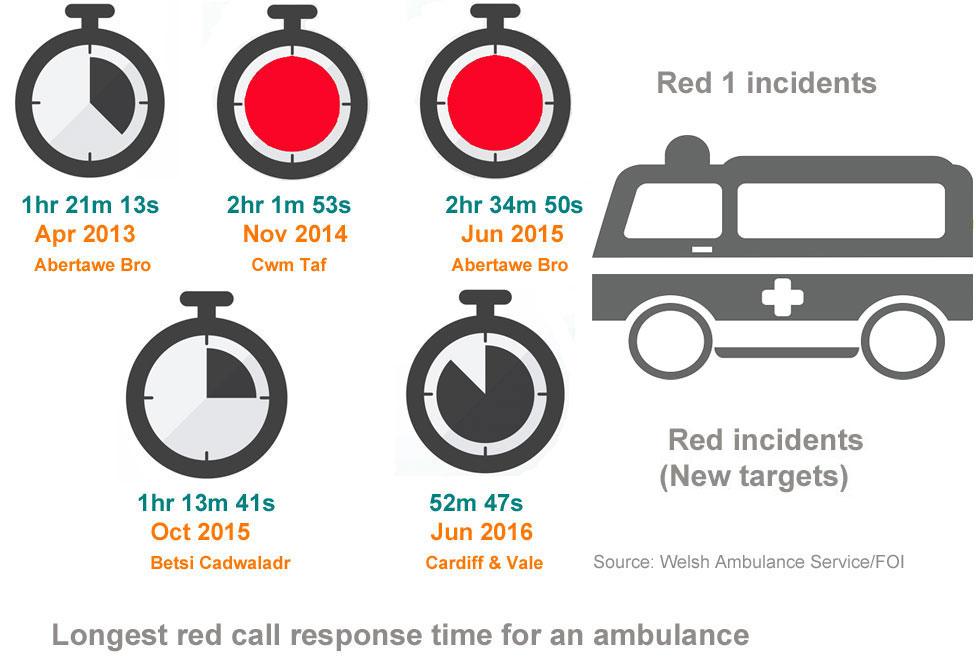
Before the changes, the worst example of a delay was more than two and a half hours
Since the new system came into force there has been a significant reduction in Wales in the length of longest waits for an ambulance response and the proportion of the most critical calls taking longer than 12 minutes.
Even in the busiest month this year - March - the proportion of red calls taking more than 12 minutes was 16.6%, down from 19% for the same month in 2015.

FATHER AND SON ON THE FRONTLINE
A day on call with father and son ambulance crew Osian and Aron Roberts
Osian Roberts is a paramedic with 25 years experience and a team leader at the Welsh Ambulance Service, working out of Llandudno Junction, Conwy county. Driving the ambulance is his son Aron, an emergency medical technician.
We spent the day with them - a 12 hour shift, which involved in two cases waits of 20 minutes outside Glan Clwyd waiting to transfer patients.
Aron Roberts said: "The hospitals are starting to fill up slowly now and we're starting to wait a bit longer outside. It's quite frustrating when you have a poorly patient on board and they need hospital treatment - it's difficult just to wait outside and wait for a bed to become available."
The day before, their ambulance was waiting outside the hospital for up to four hours before patients could be taken in.
"We can take patients to get scans and X-Rays but it's not our role to do that, it should be the hospital's," he said.
"We're sat here thinking someone needs our help and can't do anything, we want to go but we just can't. When I first started I thought I'd be going to road accidents and cardiac arrests but I'm seeing more of the older generation."
Osian Roberts said the job had changed a great deal.
"When I started more than 25 years ago, it was life or limb emergencies. Now we're going to more calls for chronic illnesses, the work is so much more diverse now," he said.
But he said there were still too many calls coming in when using a GP or pharmacist might be a better alternative.
"The public need to be educated to choose well before they call the ambulance. Think wisely before you call - there are other options - unless it's a real emergency of course, then call 999," he added.
"It's possibly the non-emergency calls which tie us up the most. We still have to turn up, we don't just leave them there, it might be making a call to their GP or getting referred to a specialised unit. It still takes time and takes resources away from the proper emergencies."
Aron Roberts added: "The other day I went to a lady with swollen knees - she didn't think of seeing a doctor but thought an ambulance would be appropriate. We're supposed to be for life and death emergencies.
"But since the transition, I've noticed the red calls are genuine red calls - and those who don't need so much of a fast response, we are still getting to them and they are getting the help they need but it's the right resource at the right time for that patient."

Darren Millar AM (right) said some suspected heart attack patients are not included as the most urgent 999 calls
But the Conservatives claimed some patients with potentially serious problems - such as chest pains - might not be getting a quick enough response because the red category was now too narrow.
Clwyd West AM Darren Millar said a constituent in Llandudno had to wait 35 minutes for an ambulance after collapsing with a suspected heart attack but he found it was not classified as critical because the patient was not unconscious.
Conservative health spokeswoman Angela Burns said: "The real scandal here is that the Welsh Government only time-targets 4% of ambulance calls, which betrays an incredible lack of accountability, particularly where conditions such as heart attack and stroke depend on the speed of treatment."
Dr Brendan Lloyd, the Welsh Ambulance Service medical director, said: "Calls in our amber category are those where the patient requires a blue light response and urgent specialist medical attention - this includes chest pain and stroke.
"For some conditions, like stroke, there is strong evidence to support a specialist treatment within a few hours of the onset of symptoms, rather than minutes."
Stephen Harrhy, chief ambulance services commissioner for NHS Wales, explains how 999 calls are continually assessed after they come in
Plaid Cymru said the Welsh Government "could not hide" behind the statistics which were only recently set and were not comparable as all nations measure urgent calls in different ways.
The party's heath spokesman Rhun ap Iorwerth AM said paramedics had told him of the stresses of dealing with the 96% of other calls.
He added: "Figures for how many hours ambulances have to wait outside hospitals before patients can be admitted to A&E are alarming.
"The figures published today for 2016 only go up to August and already they're nearly as high as for the whole of 2015."
Stephen Harrhy, chief ambulance services commissioner for NHS Wales, is responsible for reviewing performance.
"Not only have we seen significant improvement but we've seen that achieved gradually over a period of time," he said.
"It has been sustained and that's really important because patients with immediate life-threatening conditions need to get an ambulance as quickly as they can."
He said the service was working with hospitals to tackle "complicated" handover problems.
This included a more coordinated winter pressures plan and introducing an immediate vehicle release policy, so ambulances waiting outside hospitals could be back on the road when the service was short of vehicles.
- Published30 November 2016

- Published27 July 2016

- Published27 July 2016

- Published31 August 2016

- Published27 July 2016
