Contaminated blood inquiry: Paul Summers given same Factor VIII batch as Aids patient
- Published

Paul Summers died in 2008 after his hepatitis C infection caused liver cancer
The father of a haemophiliac, who was not told he had been infected with HIV and hepatitis C, said his son was given blood from the same batch as a patient who died of Aids.
Paul Summers, from Llantwit Major, in the Vale of Glamorgan, died in 2008.
His father Tony was shown a letter, showing he received the same batch as a patient, whose name was redacted.
The public inquiry into the UK-wide blood contamination scandal is hearing evidence in Cardiff.
Mr Summers, 83, said it was "quite clear" that the redacted name in the letter - contained in Paul's medical records - was that of a 23-year-old man from Cardiff who was the first UK haemophiliac to die of Aids in 1983.
That unnamed Cardiff patient, given Factor VIII blood products, and a Bristol man were among the first 20 Aids cases reported in the UK that summer.
Paul died after his hepatitis C infection caused liver cancer, in December 2008, aged 44.
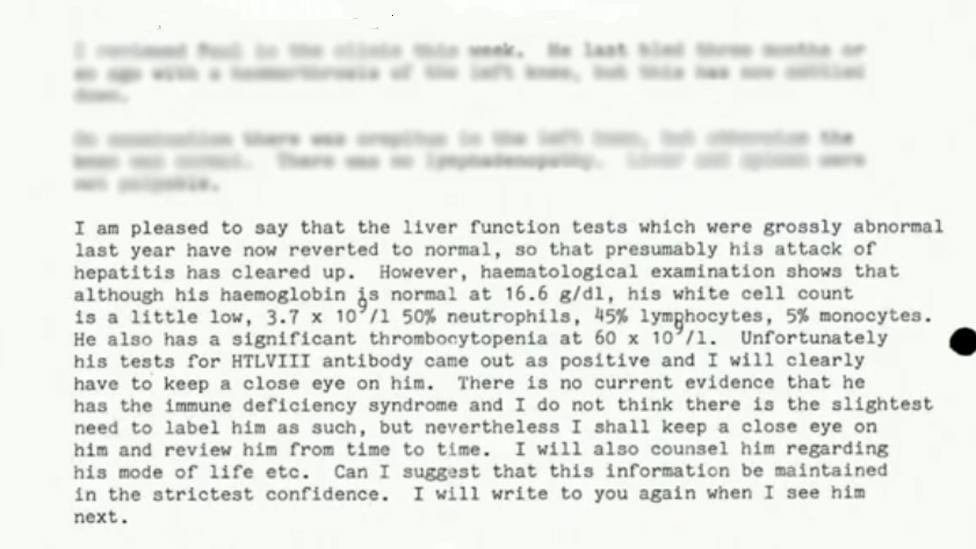
A letter from Prof Bloom to Paul's GP in 1985, which shows that he was HIV positive - HTLVIII - but it was not shared with Paul
Documents from Paul's records - only obtained by the family last year - revealed that haematologist Prof Arthur Bloom communicated Paul's positive test for HIV to his GP in 1985 - but Paul wasn't told.
Paul only found out he had HIV in 1986 when his new doctor at Derriford hospital in Plymouth - where he had moved to, to study architecture - asked him how he was handling it.
The doctor then wrote to Prof Bloom - based at the University Hospital of Wales in Cardiff - to say Paul had been "apparently unaware" he had the virus and asked if this could be correct.
But Prof Bloom responded to say he had been "counselled extensively" and had been advised "in some detail" about sexual practices.
Mr Summers said Paul recalled there had been a brief discussion about sexual practices but he had no idea why and that it was untrue of Prof Bloom - who died in 1992 - to suggest Paul knew.
"No-one had told him he had HIV and it had not occurred to him that this is what they were talking about."
Mr Summers said when he met him in Plymouth to discuss the diagnosis, Paul was "visibly shaken" but wanted to get on with his course and become an architect. "He was quite a strong character, he simply got on with it."

Paul's father Tony and wife Monica giving evidence
Paul met his future wife Monica, an American exchange student, when he started his course in Plymouth. They kept in touch by phone and letter, but he told her of his HIV diagnosis on a trip to the United States in the summer of 1988.
They married a year later and set up home in the UK, with Paul, having earned a first class degree, working as an architect in Bristol and then Cardiff.
Monica flew over from America, where she now lives, to give evidence to the inquiry.
"I always say that the HIV and haemophilia was certainly a part of our life but that wasn't our life," she said.
"We had to live with these but sometimes we had moments of reprieve."
'I feel guilt that we allowed it to happen'
Monica also shared her experiences of the liver transplant Paul went through in 2008 after the hepatitis C virus caused him to develop liver cirrhosis.
She said the day of the transplant was "going to be the day we got out life back".
But Paul died a week later.
Finishing evidence, Tony Summers said: "I think we've reached the end of the beginning and I think this is the beginning of the end, and more than anything else I want to live long enough to see it."

Paul and Monica on their wedding day in November 1989

Paul and Monica Summers with their daughter, who was five when he died
Monica ended her evidence by reading out statements from several of Paul's friends, colleagues and clients, as well as their adopted daughter.
Their daughter's statement said: "The realisation that there are still years ahead until we have the answers we need are daunting to say the least."
Sir Brian Langstaff, the chairman of the inquiry, told Monica she "painted not only a compelling picture but a much more vivid picture of what Paul was like than could ever be represented in words".
At least 300 people in Wales are known to have been infected, but this does not include others who have died or may not have known they were infected.
'We just felt there was a cover up'
A woman whose father died after contracting hepatitis and asbestosis after a blood transfusion told the inquiry she was asked to cover up details of his death at the University Hospital of Wales in Cardiff in 1972.
The woman, who was granted anonymity, said her father, a plumber in the docks, and family had not been told of the diagnosis before his death,
She said one nurse told her: "Things are happening here. I can't stay here anymore."
She said she was told by a nurse they could not carry out the post mortem examination because the room would have to be closed for three days and fumigated for asbestosis and hepatitis.
"'Would you accept leukaemia on his birth certificate even though that's not what he died of?'" she was asked.
"We felt the nurses knew more than what they were able to say," she said.
"They knew he had it, they told us. I think some of the nurses got terribly upset by what was happening in the background.
"The things we didn't know. It was the 'why'? Why didn't they put the details on the death certificate? We just felt there was a cover up."
On finishing her evidence, the woman said "I would like to thank the inquiry for bringing this to the fore and hope something good can come out of it and these cover ups won't keep happening."
Sir Brian thanked her for the "clarity" of her evidence.

Jane Jones believes she was infected with Hepatitis C in 1982
'I just wanted to die'
Jane Jones, who is from Groeslon near Caernarfon, Gwynedd, has Von Willebrand disease - a blood clotting disorder. She believes she was infected with hepatitis C in 1982 after being given cryoprecipitate - a frozen blood product - after a miscarriage.
She was diagnosed with hepatitis C, which her mother also had, in 1992, after her health started to deteriorate.
Ms Jones explained she had her gallbladder removed in the early 1990s and no staff in the surgical ward would bring her food because they were scared of the infection.
She said: "They treated me like I had the plague. My parents and children came to visit me dressed in masks."
Ms Jones described liver problems and also the effects of interferon and ribavirin treatment, which on the third series without success had led to her contemplating taking her own life and a short spell in hospital.
"I had suicidal thoughts," she told the inquiry. "I just wanted to die. It destroyed my white blood cells, I lost all of my hair."
"Apparently a few people had committed suicide while on the treatment because it's so bad. It takes hold of you. I just didn't want to carry on."
Ms Jones then found out in 2004 she was high risk for variant Creutzfeldt-Jakob disease (vCJD), which she said was "another knife in my heart".

After her transplant, Jane Jones has been able to enjoy trips with her children and grandchildren
Ms Jones also had to have a liver transplant, which was successful. In 2014, she cleared the hepatitis C virus.
At the end of her evidence, she paid tribute to her partner Johnny and her "donor angel".
Sir Brian thanked Ms Jones for "not sparing us the brutal reality of your illness and the treatment you have had".

'This is still hanging over me'
The inquiry also heard from a severe haemophiliac who was infected with HIV and hepatitis C.
He described his brother - who died of Aids in 1992 - as the "bravest person I've ever met in my life".
The man, granted anonymity by the inquiry, said his brother was deliberately placed on a placebo while he was given the anti-HIV drug AZT, so doctors could assess its effectiveness.
He said there were times he didn't think he could visit his brother because of the guilt he felt over the condition he was in.
Both often shared batches of blood products when they were children to treat their severe haemophilia.
He said he and his wife were told in 1983 to terminate the pregnancy of their son by Prof Bloom to reduce the risk of passing on haemophilia.
When asked if he thought he had been asked to terminate the pregnancy because Prof Bloom thought there was a risk he could be passing on HIV to the unborn baby, he said: "Absolutely."
After he was officially diagnosed in 1984, the man's wife was pregnant with another child, which they chose to terminate.
He said when he and his brother were diagnosed with HIV at the same time, both were asked "not to tell anyone".
"It still hangs over me now," he said. "The HIV is under control, I've now cleared hepatitis C, but this is still hanging over me."
- Published25 July 2019

- Published22 July 2019

- Published24 July 2019
- Published15 February 2018

