Coronavirus: Community oxygen tests 'key to second wave'
- Published

These £50 devices are being developed in south Wales to test oxygen levels
Oxygen levels in suspected coronavirus cases should be monitored in the community to help hospitals cope with a second wave of cases, according to Wales' leading respiratory doctor.
Dr Simon Barry said early on in the pandemic it became clear reduced oxygen levels in the blood suggested a patient had Covid-19.
But flu and pneumonia will be more common in a future winter peak.
This means more community monitoring would be needed, he said.
Dr Barry is leading the implementation of Welsh guidelines to treat the virus, and said work was under way to conduct specific tests before coronavirus patients were admitted to hospital in future.
Most people with coronavirus only have mild symptoms, and sometimes none at all.
But doctors report low blood oxygen saturation levels among those who are admitted to hospital with coronavirus.
Healthy adults usually have saturation levels of between 94% and 99%, whereas those with Covid-19 can fall below 90% and require oxygen therapy and, in some cases, ventilation in intensive care.
Dr Barry, who has treated Covid-19 patients, has also developed a website that delivers the latest treatment guidelines to doctors in all Welsh hospitals.
He said: "Early on there was a clear recognition that this disease caused oxygenation failure in people who presented.
"The ones who got sick (the 20% of patients who get sick) had low oxygen levels and they came into hospital with low oxygen levels."
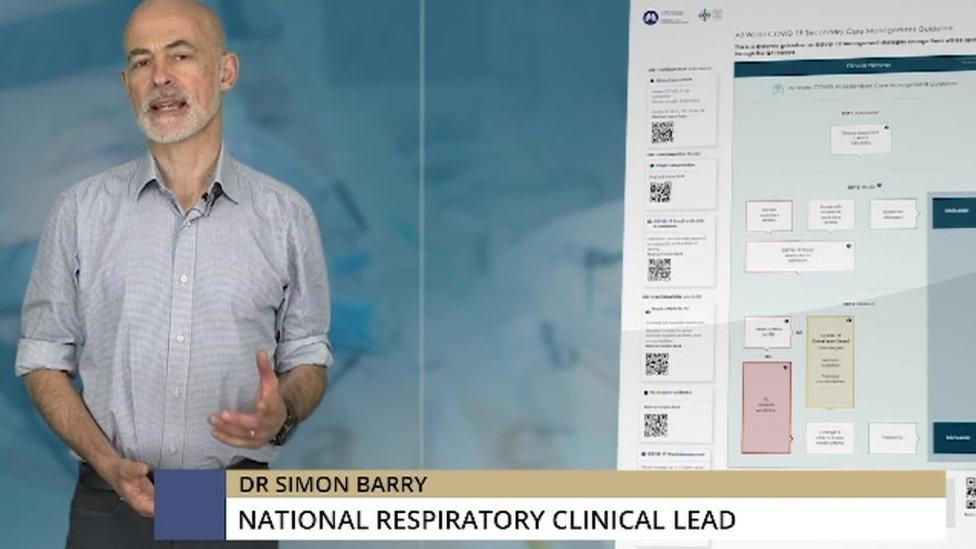
Dr Barry has been producing online training videos for doctors
Dr Barry said far more patients had been treated with a continuous positive airway pressure (CPAP) device than he had anticipated.
The treatment, which involves a tight-fitting mask that delivers a continuous flow of oxygen, is given while the patient is awake and does not require them to be sedated and placed on a mechanical ventilator.
"We've learned that actually you can manage patients with quite bad oxygenation failure on the wards, using CPAP, and getting them to lie on their front," he said.
"And we also know that, if you go to ITU [an intensive therapy unit] and you're ventilated, you have very high mortality. It's about 70% if you're actually invasively ventilated."
Early intervention is key in providing the best treatment, and monitoring blood oxygen levels could prove crucial in determining whether someone has coronavirus or another respiratory illness.
Dr Barry, who is based at Cardiff and Vale health board, said a winter surge would mean Covid-19 mixing with flu and pneumonia cases.
That, he said, would mean it would be "extremely difficult" to manage patients into "safe streams" within hospitals, making community testing necessary.
"We are looking at a mechanism to be able to do all of these specific tests, point-of-care, in the community. Both in primary care but also using the Welsh ambulance crew, so they will be able to make a specific diagnosis within minutes."

The oximeter is being developed at labs at the University of South Wales
Engineers at the University of South Wales have received Welsh Government funding to create a new oximeter, a £50 portable device which can accurately measure a patient's blood oxygen levels.
Prof Nigel Copner, who has led the programme to rapidly develop the oximeter at the laboratory in Treforest, said the devices would be ready "in weeks" and Welsh patients would be the first to benefit.
"Wales obviously has first call, the Welsh Government has funded the project in total. And we have contract manufacturers down in Sony that can manufacture the device and turn it around very quickly."
Prof Copner said the device had "no issues" with pre-existing supply chains, which have been stretched by global demand.
"We can actually manufacture and build this device very easily in south Wales, and we can turn around high volumes in a matter of weeks," he added.
Clinicians have also responded in innovative ways during the pandemic.
Dr Barry said a pioneering online training platform had helped Welsh doctors to provide the best treatment, as lessons were learned and best practice shared quickly with colleagues.
"Traditionally in Wales we have seven health boards that do things in seven different ways," he said.
"But if you stood above it and you look down, it's an enormously inefficient and ineffective way to manage cases.
"We're trying to rise above that by saying 'look, this is the national guideline'. We are getting experts within Wales who are talking about updates and talking about what should be the best practice. And that seems a logical way to proceed."
- Published30 March 2020

- Published7 April 2020
- Published16 April 2020
