NHS Wales records its worst ever performance figures
- Published
- comments
NHS Wales: 'No ending sight for exhausted GPs'
The NHS in Wales has recorded its worst performance figures ever amid growing concerns on staff pressures ahead of a difficult winter.
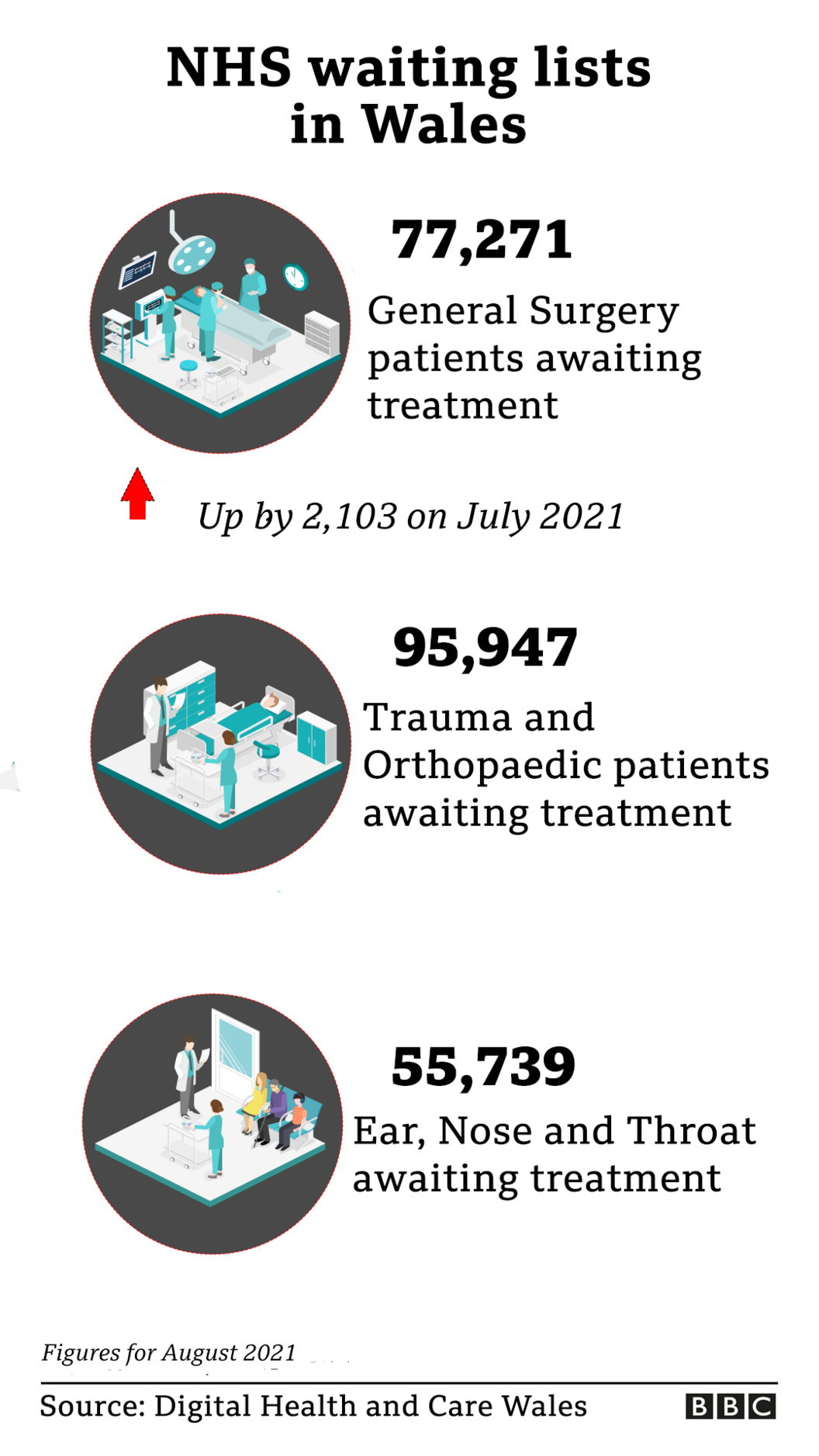
Nearly 250,000 people have been waiting more than nine months for treatment, up from about 25,000 at the start of the pandemic, statistics show.
NHS Wales chief executive Andrew Goodall said the system was running "at the hottest we've seen" due to Covid.
It comes as the Welsh government unveils its winter pressures plan, external.
The Welsh Conservatives criticised the plan as a "copy and paste failure" from last year.
Russell George MS, the party's health spokesman, said the party had called on the government to "bring in rapid diagnostic centres to spot cancers earlier and deliver treatment to patients closer to home", which would "help address the backlog".

Almost two-thirds of Welsh NHS staff surveyed said they felt tired or exhausted
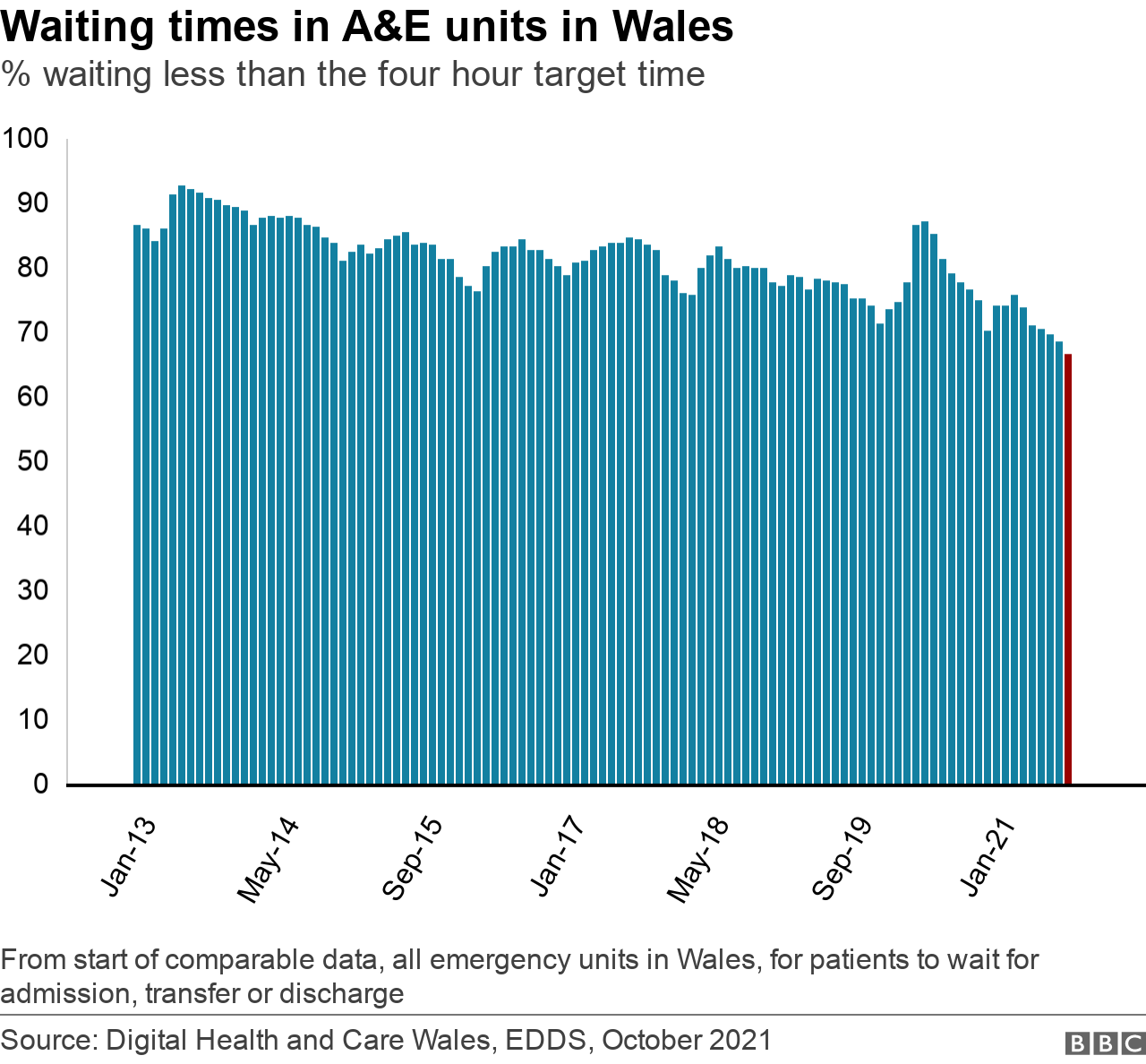
Latest Welsh NHS data shows accident and emergency waiting times were again the worst on record - only 66.8% were admitted, transferred or discharged within four hours.
This was down from 68.7% in July, which was itself a record.
Cancer treatment waiting times have improved slightly since July - 63.2% of patients newly diagnosed with cancer started their first treatment within 62 days of first being suspected of cancer. This is one percentage point higher than August 2019.
Seventeen organisations representing staff have jointly warned of a "deepening winter care crisis".

Dr Goodall said: "It does feel like this is the most challenging period... and we can see that in the data.
"Rather than just focusing on coronavirus we've got the NHS trying to restore a range of activities across all its settings."
Dr Goodall said there were 700 Covid patients in hospital beds - the equivalent of two medium-sized district general hospitals - alongside record ambulance calls, high levels of emergency demand and a busiest-ever primary care sector.
Wales' newest hospital, the Grange in Cwmbran, for a second month in a row recorded the worst A&E performance in a month for any Welsh emergency unit with just 38% of people dealt with within four hours. The target is 95%.
And 8,484 people waited more than 12 hours in A&E when the target is that no-one should wait that long.

Routine surgeries have been delayed because of the pandemic
Waiting lists also grew further to 657,539, a record which is equivalent to more than 20% of the Welsh population.
Dr Goodall said some planned operations would likely be postponed over the winter.
"Inevitably there will be some disruption and that will involve planned care, but the commitment of the NHS is to maintain as many of its activities in all of its settings for as long as possible," he said.
He said health boards would need to make decisions regarding the extent planned services could be protected in the face of other pressures.
Earlier this week, Health Minister Eluned Morgan said it would be "very tough" to work through waiting lists, but health boards had been told to "keep in touch" and offer support, such as pain relief, to those waiting.
The Welsh government's winter pressures plan includes an extra £40m for social care, as well as extra funding for front-line services, to try and tackle delays discharging patients from hospital and cut readmissions of frail and vulnerable people.

Dr Andrew Goodall said he was concerned about the resilience of the care sector
But Dr Goodall said staff shortages in the care workforce were concerning.
He said: "The resilience of the care system is a concern - it feels it is at its most fragile even with the support available.
"We've provided funding to make sure the care sector is further supported, but workforce elements is a problem, whether it's people choosing to enter a care career or the community prevalence of Covid, meaning staff have to self-isolate."

Dr Alice Groves is expecting it to be the hardest winter in the health service's history
In an effort to take pressure off emergency services, Aneurin Bevan Health Board has set up urgent care centres at Newport's Royal Gwent Hospital and Abergavenny's Nevill Hall Hospital.
This was after estimating that between 30% and 50% of those attending A&E could be seen in primary care settings.
Already, 5,500 patients have been seen and clinical director Dr Alice Groves said: "The worry was patients would have waited ages at A&E or become unwell trying to access other services."

Exhausted staff
Allow X content?
This article contains content provided by X. We ask for your permission before anything is loaded, as they may be using cookies and other technologies. You may want to read X’s cookie policy, external and privacy policy, external before accepting. To view this content choose ‘accept and continue’.

Meanwhile, 17 medical royal colleges and faculties have warned of a growing winter crisis and called for a national plan to deal with staff shortages.
A recent survey by the Royal College of Physicians found 46% of respondents in Wales said their organisation was not at all prepared for winter, 37% felt personally unprepared, with 63% feeling tired or exhausted.
Asked if the pressures of winter might "break" exhausted staff, Dr Goodall said: "This [pandemic period] has been a much more sustained experience than many of us would have envisaged.
"When we usually talk of a major incident we talk of a matter of hours or days. We've been running a major incident situation for 20 months now.
"Everybody needs to do their bit including the public, but I know NHS staff will pull out all the stops."
WONDERS OF THE CELTIC DEEP: Encounter mythical coasts and extraordinary creatures
POETRY FOR PLEASURE : A mirror to reflect the most deep and difficult to articulate feelings

Related topics
- Published13 October 2021

- Published23 September 2021

- Published21 September 2021

- Published28 May 2024
- Published17 June 2021
