NHS Wales: Patients can be sent home without care package
- Published

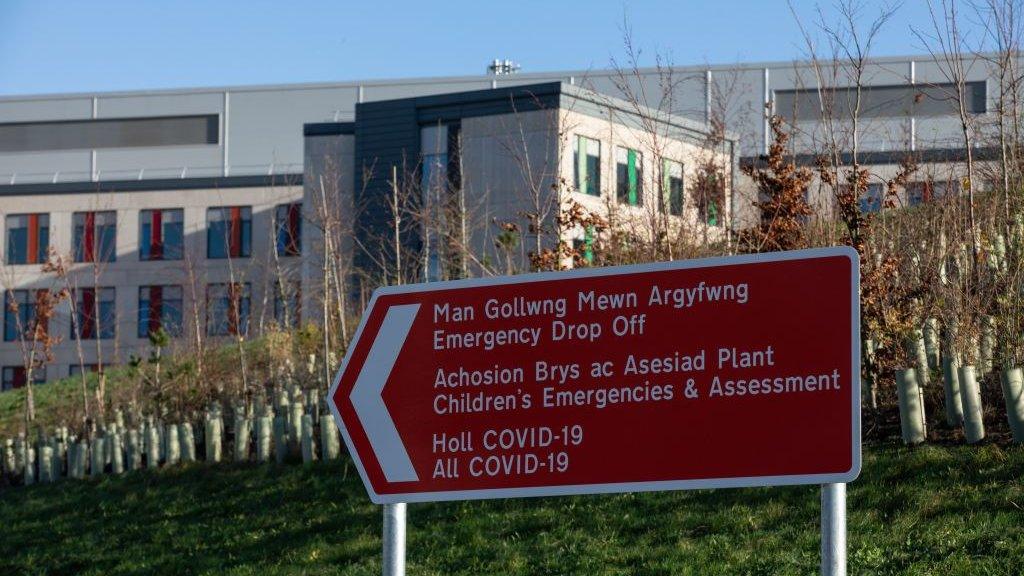
Health boards across Wales say they have hundreds of patients well enough to leave
Senior NHS staff have been advised by the Welsh government to discharge people who are well enough to leave, even without a package of care.
But one GP called the announcement "terrifying" and warned that patients could deteriorate and end up back in hospital.
The seven health boards in Wales have nearly 1,800 patients medically well enough to leave hospital.
The Welsh government has called the NHS situation "unprecedented".
The message comes after one health leader said the NHS was on a "knife-edge" in terms of its ability to cope.
The letter from the chief nursing officer and the deputy chief medical officer to the health boards offered "support and advice to ensure patients are kept as safe as possible, and services are kept as effective as possible over the next period".
It said the NHS was facing exceptional pressure and there were more than 500 confirmed Covid cases in Welsh hospitals, with rapid increases in other respiratory viruses.
"We recognise that day to day clinical decision-making must adapt to these exceptional pressures, to ensure the NHS resource is being used for the greatest benefit.
"Our hospital capacity must be preserved for those at greatest risk with the greatest chance of benefit, this will require us to make every effort to keep people at home, not to admit people to hospital, unless absolutely necessary, and to return those in hospital to their homes or alternative place of safety as quickly as possible."

The Welsh government advises health boards to discharge patients well enough without a care package
An NHS care package offers means services to patients in their own home or in a care home.
This could mean care from a community nurse or therapist, for instance in their own home. In a care home, this could mean fees being paid.
Dr Sayma Ahmed, a GP at Cloughmore medical centre in Splott, Cardiff, told BBC Radio Wales Breakfast that people usually needed carers to take their medication, feed them, help them go to the toilet, and if a plan was not in place they would eventually deteriorate and end up back in hospital.
"I completely understand the thinking, I've worked in a hospital for many years before becoming a GP, it does make sense, but being on the other side in primary care directly seeing these patients in their homes, we are dealing with them day to day.
"There are lots of patients we have to send in because they have got to a state where they had to go in [to hospital] because they haven't been able to care for themselves, and essentially they've become unsafe, or are already unsafe, so it is terrifying, and I can understand people asking what are we going to do, but this isn't going to fix it."

Dr Sayma Ahmed has been a doctor since 2010, and says this is the worst winter she has experienced
The letter added that it offered support and understanding, as this necessary adjustment in the clinical risk threshold for hospital care may be concerning for some professionals.
'Arrangements... may not be perfect'
It said that "the NHS will serve our population best if as many people as possible either remain at home or return home from hospital care as quickly as possible".
It went on that "there will be a need for everyone to consider discharge arrangements that may not be perfect, a care package may not yet be in place, and social assessments may need to happen at home rather than in hospital".
Mary Wimbury, chief executive of Care Forum Wales, said the social care sector and health sector need to work together to make the system work.
"We have got to be more joined up in terms of paying appropriate rates, most care in Wales is commissioned by health boards or local authorities, they've got to be paying enough, so that social care providers can actually pay their staff to sufficiently retain and recruit them and provide the support that people need."
She added that there were two types of care packages, one for care home residents, and the other for people who can live at home but need carers to come in, and that a care package was "absolutely vital".

Mary Wimbury says health boards needed to recognise their own attitudes in terms of how they commission care, and how they pay for it is causing that crisis
"We can't be in a position where we are just leaving people to just fend for themselves, we've got to provide that care, but we've got to provide the support for the care workers.
"It is a lot cheaper for people to be cared for in their own homes than in hospitals, and this can free up money to invest properly in social care, which will keep people out of hospital in the first place, and get them out more quickly when they are there."

Lots of things are contributing to the current pressures.
The first week of the new year is often one of the most difficult for the health service, with services, during Christmas and the other bank holidays, not running at 100% capacity.
Some might also have delayed getting their illnesses checked out during this period, to avoid the risk of not being able to spend the festive period at home or with their loved ones, but their conditions will not have gone away.
For the first time since the start of the pandemic flu is back in quite a big way, affecting staff as well as patients, and Covid is still a threat.
But I would treat with a degree of suspicion anybody who sought to claim that the impact of winter illnesses was solely to blame for the current crisis.
What we're seeing is evidence in real-time of the NHS's inability to cope with all the demand coming in, whatever the reason for that demand.
And although the pandemic and its after-effects have worsened the situation, this is a pressure that's been building for years.
It involves questions about funding, staff levels and whether the social care system is fit for purpose in dealing with the demands of an aging population: a population whose needs are so much different now to when the NHS was established 75 years ago.
And quick fixes won't solve those huge underlying issues.

Swansea Bay health board said it had nearly 280 patients who were medically well enough to leave - the equivalent of 10 wards - but could not for a number of reasons.
The health board said it was urging families to help free beds by supporting relatives to go home, which was also to ensure patients ready to leave were kept safe, and given the best chance to recover.

Wales' largest health board, Betsi Cadwaladr declared a critical incident on Tuesday and said staff are forced to deal with overcrowding in the department
The six others - Betsi Cadwaladr, Cardiff and Vale, Aneurin Bevan, Hywel Dda, Cwm Taf Morgannwg and Powys, said they had 197, 289, 253, about 300, almost 400 and 24 respectively.
The figures come as most health boards across Wales said they were facing extreme pressures.
A Welsh government spokesperson said: "The NHS is facing unprecedented demand this winter responding to both flu and Covid cases, and we have asked health boards to focus on safely discharging those who no longer require hospital care.
"In some cases this may involve being cared for at home, and we have asked for family and loved ones to help where possible, to free up beds for people who require urgent care, we have already made more than 500 extra community beds and packages of care available this winter to help discharge people from hospital, and are working on delivering more."
- Published4 January 2023

- Published3 January 2023

- Published2 January 2023

- Published31 December 2022

- Published30 December 2022