NHS Wales on a knife-edge says confederation leader
- Published
- comments
A long term plan for health and social care is needed to ease pressure on the NHS, it's been claimed
Tough choices have to be made now to protect the NHS, a health leader in Wales has warned.
Darren Hughes, director of the Welsh NHS Confederation, said the NHS is on a knife-edge in terms of its ability to cope.
A consultant for Wales' largest health board, which has declared a critical incident, said staff are forced to deal with overcrowding in the department.
The Welsh government called the situation in the NHS "unprecedented".
Mr Hughes, said the NHS was already struggling to cope, and the Christmas period had "tipped it over the edge".
"In the run-up to Christmas there were multiple hospitals across Wales, across all health boards pretty much who were at the very highest level of pressure having to postpone care and treatment for people who were really needing it."
He said this was down to staff on sick leave and annual leave, but also the impact of Covid and flu.

Mr Hughes said there was as staffing crisis in the hospital sector as well as the social care sector
Mr Hughes said politicians needed to commit to a long-term plan to put these things right.
"The NHS has been under pressure and under-funded for a significant period of time, we've got a political blame game happening between Cardiff and Westminster.
"What we are seeing across the UK, the NHS in Northern Ireland, in Wales, and in England, is pressures that simply cannot be coped with.
'Toughest times'
He said it was much more than just an investment in beds, but to develop the workforce so that there is the staff which "we simply don't have at the moment".

Nurses across Wales staged their first strike on 15 December 2022
"I've been saying this for so long: the NHS is in danger, and the government aren't doing enough, tough choices need to be made.
"The NHS in Wales is in a hugely difficult situation, there's a crisis in the NHS, and there's a crisis in social care - we're facing the toughest times we've seen."
Mr Hughes said a clear sustainable funding plan and a commitment from both the Welsh and UK governments for the service to be planned better were needed.
Wales' largest health board, Betsi Cadwaladr, which covers north Wales said all routine appointments for Tuesday would be postponed, and there would be long waits for emergency care.
'Overcrowding and congestion'
Dr Phil Morgan, an A&E consultant at Ysbyty Gwynedd, described the situation as "demoralising".
"Certain things that would normally happen routinely are cancelled or postponed to make additional resource available for dealing with the situation that we have in the emergency department," he said.
"We know we can provide a better standard of care than we're delivering, but we're just forced to cope with the overcrowding and the congestion in the department.
"We don't want to be seeing patients in corridors. We don't want to be breaking bad news in cupboards... it's just the only thing we can do to keep the system going."
He said staff were "tired" from working at a "high intensity" but thanked patients for listening to their messaging after seeing a drop in the number of people turning up to A&E.
Cwm Taf Morgannwg health board said its emergency departments were under extreme pressure and to only attend if absolutely necessary.
Hywel Dda health board said its hospitals continue to be extremely busy with many sick patients and a continuing high demand for emergency and urgent care.

Health boards across Wales, including Betsi Cadwaladr are asking people to only come to the emergency department if it is a life-threatening injury, due to an unprecedented demand
Aneurin Bevan health board said it was currently at red level (defined as extreme pressures) due to demand across all its sites and services.
Powys health board said it had not declared critical incidents for its community hospitals, but it was supporting the wider system to respond to the current challenges.
Cardiff and Vale University health board said it was also facing "significant and sustained pressure" and asked the public to carefully consider which service they choose for their needs.
Other hospitals, like Morriston in Swansea, have been asking people not to turn up to A&E unless it is a life-threatening injury or illness.

Ambulances queuing outside Ysbyty Gwynedd hospital in Bangor
Kathy Cracknell called an ambulance for her 98-year-old mother-in-law, Jean Cracknell, due to a chest infection.
She said that after the ambulance took Jean to Wrexham Maleor hospital from her home in Mold, Flintshire, she was kept in overnight to be monitored.
"The nursing staff were happy for her to be discharged on New Years Eve. We talked to them at about nine or 10 in the morning and they said they were waiting for a doctor to come and discharge her.
"We went along at three in the afternoon for visiting time hoping that it had all been processed - only to be told that because of illness there were no doctors that were able to discharge patients so she had to spend an extra night in."

Cathy said her Mother-in-law got "got shuffled around and felt very confused as during the night there was obviously a shortage of beds"
Kathy said she phoned the hospital again the following morning at 10:00 GMT.
"We were told that they were happy with her condition and they wanted to discharge her, but there was still the shortage of doctors," she said.
"She was discharged at two that afternoon which is about 36 hours after she was ready for discharge."
Dr Olwen Williams, vice-president of the Royal College of Physicians in Wales said hospital staff were suffering "moral injury, external".

Dr Olwen Williams says every winter is difficult but this year is significantly harder
"The pressures on our staff are tremendous, not only are they themselves falling with influenza, vomiting bugs, and Covid, they also have to deal with the fact that there are a significant number of vacancies across both health and social care that are adding to these pressures of the illnesses that we are seeing as well."
Dr Williams works at Betsi Cadwaladr and said staff have been asked to volunteer to do extra shifts next week in order to cope with the internal emergency that has been called, but that staff were at "breaking point".
'Very serious'
Richard Stanton, a professor in virology at Cardiff University said it was "very, very concerning".
"When you hear the stories from people working in the NHS, when you look at the statistics around how long people are waiting for ambulances, how long ambulances are waiting to get people into A&E, how long people are waiting in A&E, all of these metrics I think are the worst that I can remember.
"So the situation in the NHS right now is very serious."
He told BBC Radio Wales Breakfast that in parts this was due to the spike in cases in respiratory viruses, in particular Covid and the flu, but there were other things that had tipped it over the edge.

Mr Stanton said to an extent it was a Covid hangover, but it was a conflation of multiple things
"What we have seen now for at least the last 10 to 12 years across the UK is an NHS that hasn't been funded or looked after properly, and as a result it has been run at risk for a long time now, before Covid.
"Right now the problem is Covid and other respiratory viruses, but this is something that has been building for many years now."
Mr Stanton added that if people had flu to try and manage it at home and medicate, and only go into hospital if it was an absolute emergency.
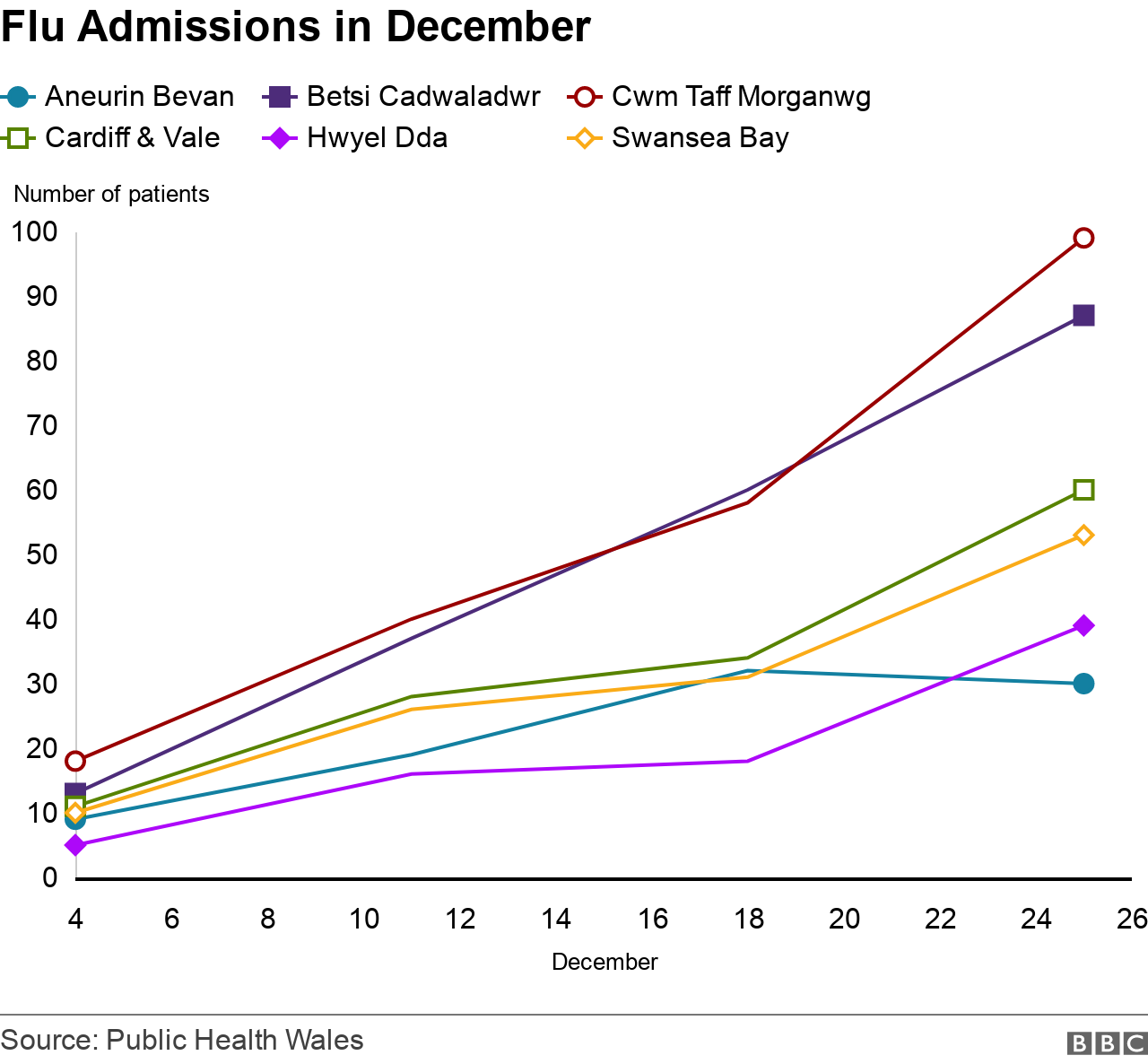
Flu hospital admissions in Wales have risen sharply over December
A Welsh government spokesperson said the NHS was facing unprecedented demand this winter responding to both flu and Covid cases, and appropriate staffing decisions would be made to mitigate risks with a focus on life-saving care continuing to be provided.
In a statement, it said anyone with flu-like symptoms should stay away from hospital "unless absolutely necessary," and asked people to use NHS 111 online website if they have a non-life-threatening condition.
- Published2 January 2023

- Published31 December 2022

- Published31 December 2022

- Published29 December 2022

- Published8 December 2022
