NHS staff shortage: How many doctors and nurses come from abroad?
- Published

The UK's National Health Service (NHS) will soon begin a major campaign to recruit health workers from other countries to meet growing staff shortages.
Reports suggest a strategy has been drawn up to target a number of countries around the world, including poorer nations outside Europe.
One estimate in March this year said the NHS will need 5,000 extra nurses every year - three times the figure it currently recruits annually.
But what about the countries that it will recruit from - what impact will it have on them?
Where do non-UK staff come from?
The NHS already recruits globally to meet its staffing needs.
More than 12% of the workforce reported their nationality as not British, according to a report published last year., external
The biggest group of foreign NHS workers are from the EU - 56 in every 1,000.
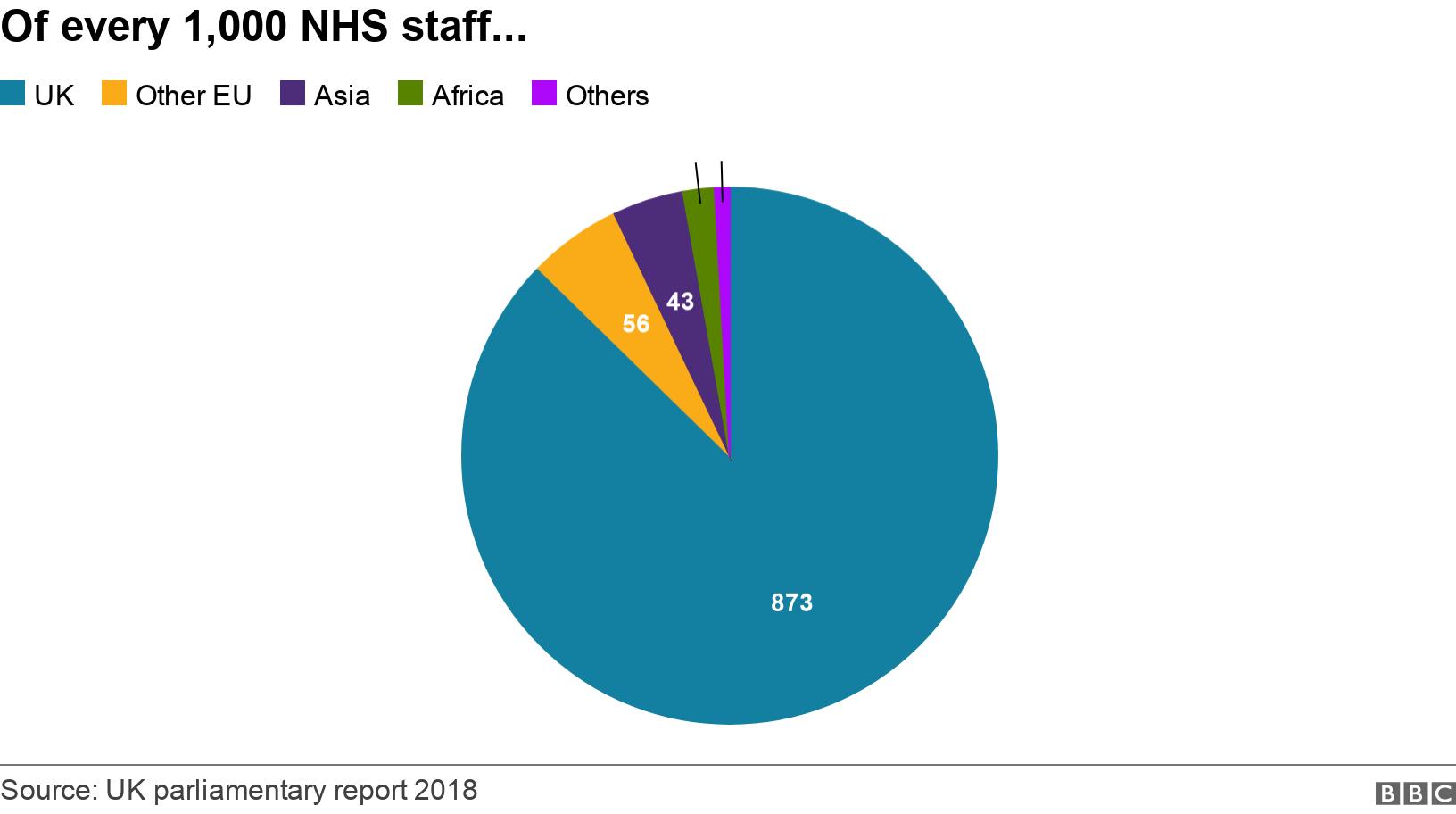
But the report noted the number of new staff coming from the EU is falling, and that this decline particularly applies to nurses.
In 2015-16, 19% of nurses who joined the NHS were from the EU.
But by 2017-18, this had fallen to 7.9%.
Which non-EU countries supply staff?
The biggest group of doctors from outside Europe is from India.
There are smaller numbers from Pakistan, Egypt and Nigeria.

As for nurses, the biggest numbers are from the Philippines and India, with smaller numbers from EU countries such as Ireland, Spain and Portugal.
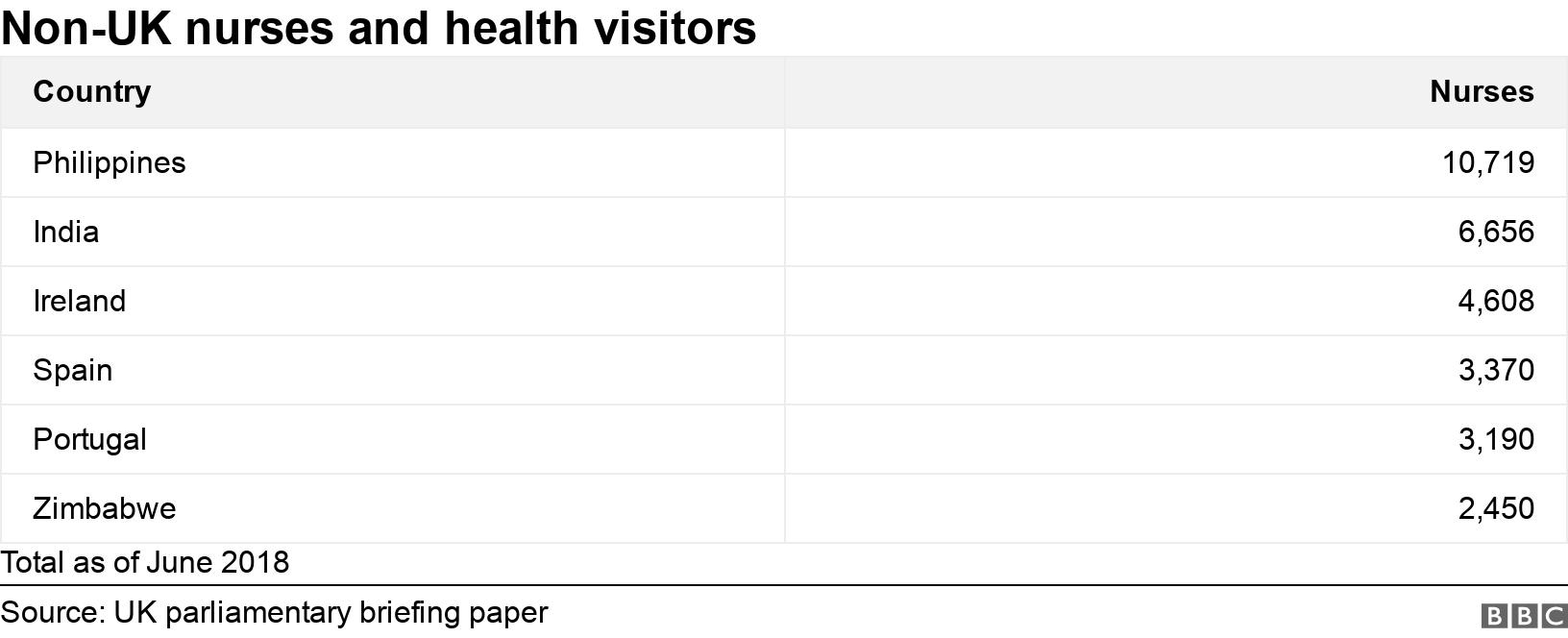
The UK regulator for nursing, the Nursing and Midwifery Council (NMC), says the numbers from outside Europe registering for the first time surged by 126% in a year., external
Between March 2017 and March 2018, there were 2,724 nationals from outside the European Economic Area (EEA) who registered for the first time.
This number went up to 6,157 for the period March 2018 to March 2019.
In the UK, the NHS Employers organisation, which handles recruitment issues, has a list of countries which it has agreed not to target because of their economic condition and the state of their health systems., external
It consists of those countries deemed eligible for aid from the OECD, the grouping which represents some of the world's wealthier nations.
There are exceptions under country-to-country agreements which allow for recruitment, such as with the Philippines and some states in India.
Nevertheless, there are staff from other countries on this list who are working in the NHS.
NHS Employers told the BBC that individuals "sometimes come to the UK independently on their own initiative without encouragement or support from the NHS."
What impact might this have?
Some of the non-EU countries which have medical staff working in the UK face significant challenges with their own public healthcare systems.
They spend far less than the UK spends on health as a percentage of GDP.
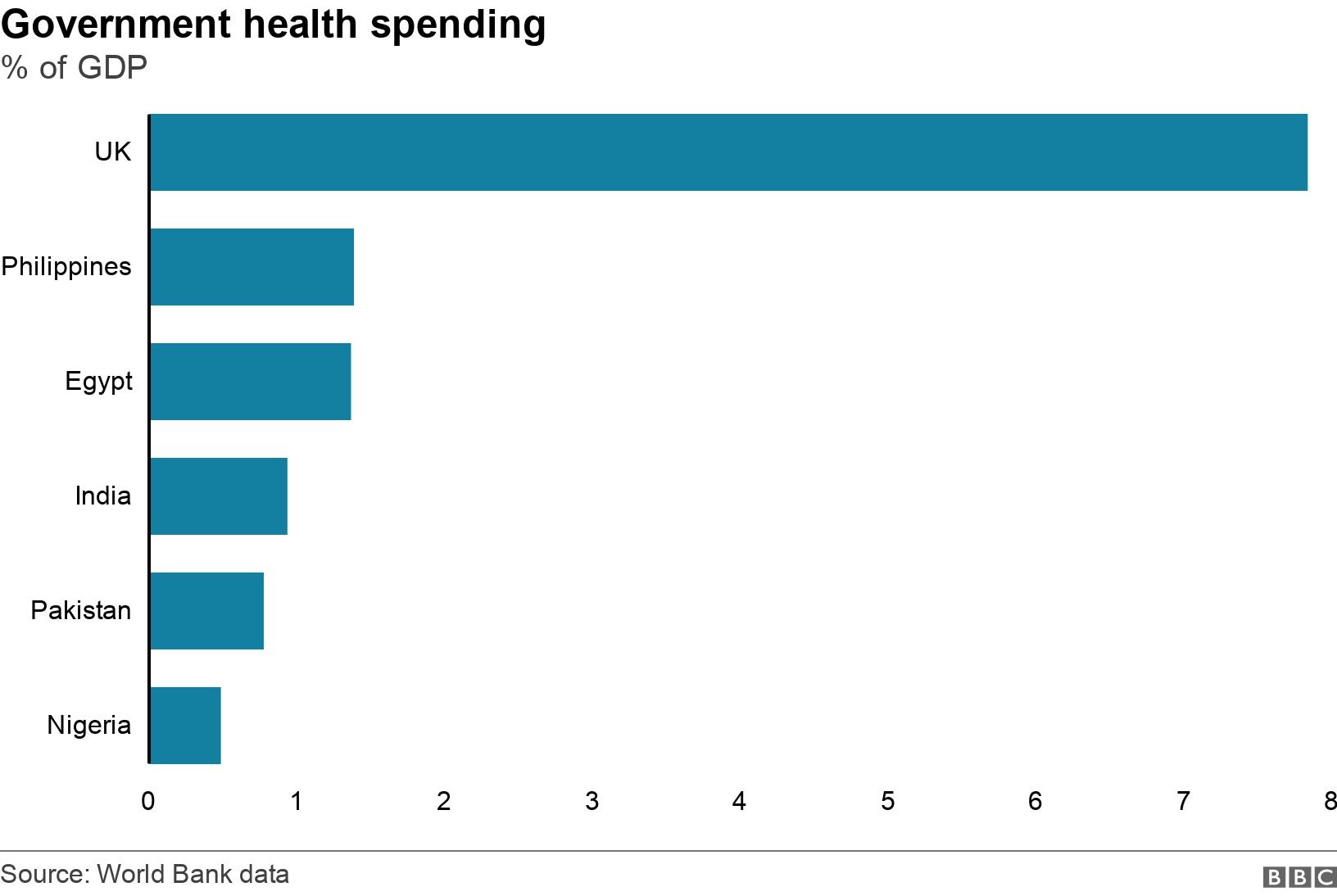
World Health Organisation (WHO) data for 2015 shows that the UK had more than 27 doctors per 10,000 people, while Pakistan had fewer than 10, and India had under eight.
As for nurses, the UK in 2015 had more than than eight nurses and midwives for every 1,000 people, while the Philippines had 0.24.
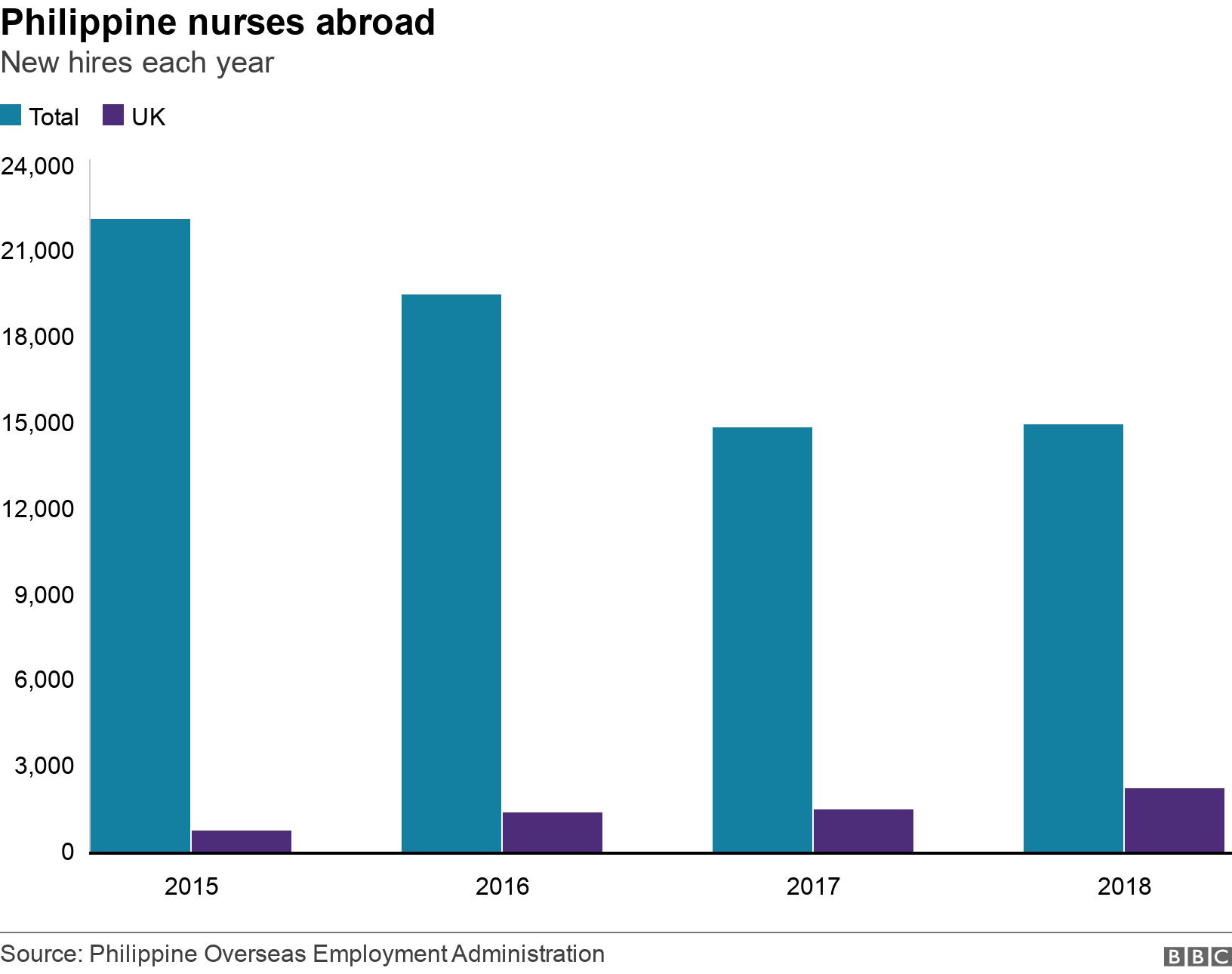
Thousands of nurses leave the Philippines each year to work abroad - nearly 15,000 were hired last year.
The number coming to the UK is relatively small, but it has been growing since 2015, according to official data.
Healthcare managers in the Philippines have been warning of growing staff shortages as a result of emigration, media reports say., external
But it's worth adding that some poorer countries whose medical staff work in the NHS, receive aid from the UK.
In 2016, both Pakistan and Nigeria were among the top five recipients of UK overseas aid.
Although much of this is spent on poverty reduction, some does go on projects to improve health infrastructure, including training health workers.
There are also projects to create better health education and awareness.
Are there any benefits for overseas staff?
Some experts believe there are benefits as well as drawbacks to the migration of health workers.
Staff who work abroad can learn valuable new skills, and contribute to their own country's economies through remittances.

Many in the Philippines are keen to get employment abroad
In the Philippines, the provision of trained medical staff to other countries is an important industry.
And in India, there's now a thriving private sector producing doctors and nurses, who sometimes move to other parts of the country to work, as well as emigrating.
Global competition for trained medical staff is increasing.
As more countries become wealthier, their populations live for longer and start to suffer from the conditions associated with ageing.
The WHO estimates that by 2030, there will be a need for more than 18m extra health workers around the world.
And it says the worst shortages will be in the poorest countries, who have increasing populations, but whose skilled professionals are seeking better paid employment elsewhere.


- Published7 January 2019

- Published14 June 2018
