Will the world's 'first male birth control shot' work?
- Published

A single preloaded syringe contraceptive shot is expected to last for 13 years
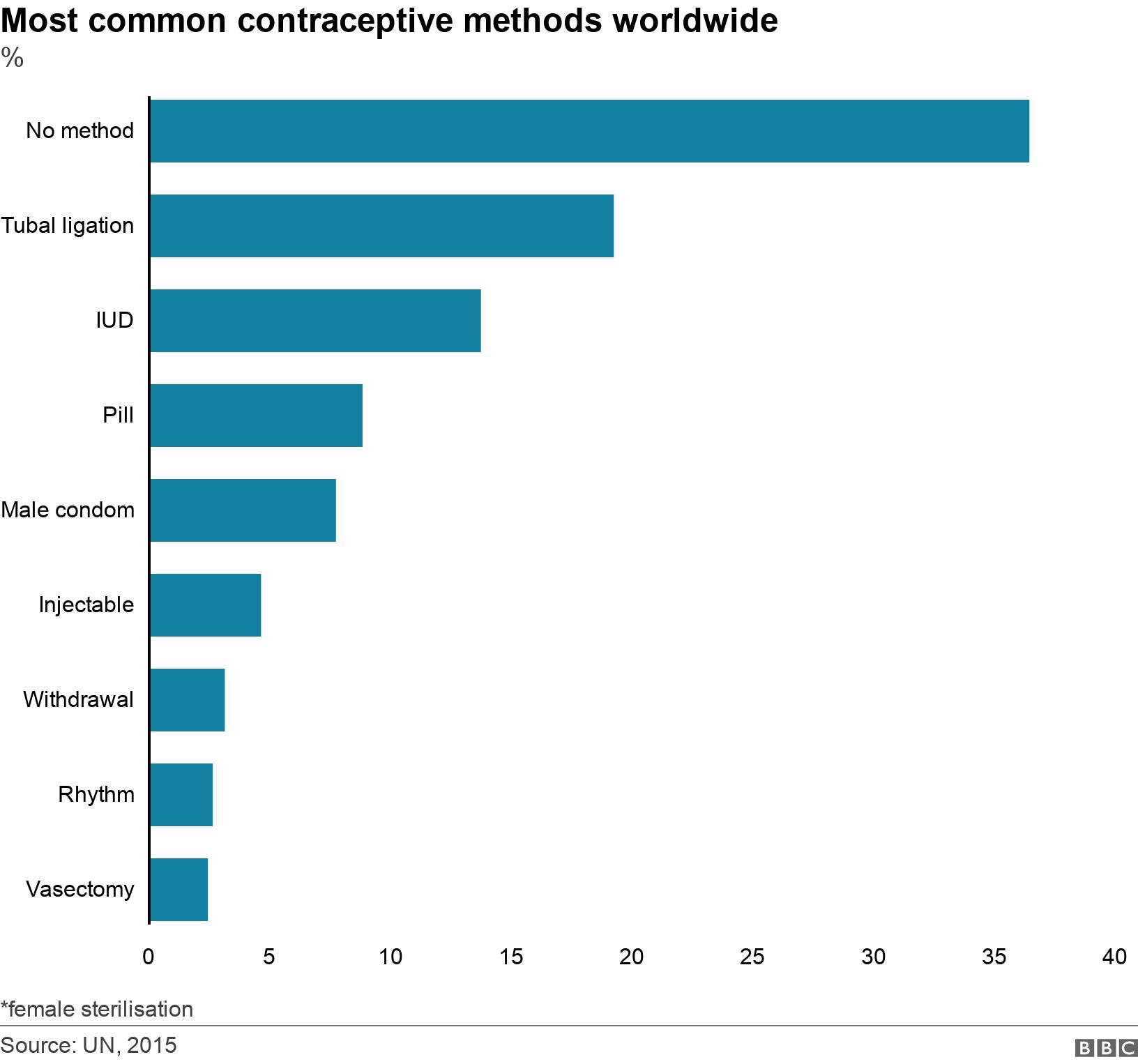
For a long time, there have been only two contraceptive solutions which rely directly on men.
They can either wear a condom, or have sterilising surgery called a vasectomy to cut or seal the two tubes that carry sperm to the penis. A male birth control pill and a contraceptive gel are still in the works.
But India says it is going to launch the world's first male birth control injection soon. Will this be the male contraceptive that succeeds?
Invented by Sujoy Guha, external, a maverick 78-year-old Delhi-based biomedical engineer, the drug is a single preloaded syringe shot into the tubes carrying sperm from the testicle to the penis, under local anaesthesia. The non-hormonal, long-acting contraceptive, researchers claim, will be effective for 13 years.
After years of human trials, the drug called Risug, an acronym for reversible inhibition of sperm under guidance, is ready. It is a viscous gel which inactivates the sperm. The effectiveness of a second part of the treatment - an injection which dissolves the gel, hopefully reversing the effects and allowing a man to father a child - hasn't yet been tested in humans, though it has worked in animal studies.
The injection inactivates sperm
And, like other non-barrier methods, the contraceptive injection wouldn't protect against sexually-transmitted infections.
"This will be a world class contraceptive for men. It is safe and effective and lasts for long. We expect it will be cleared for production in the very near future," says RS Sharma, a reproductive biologist at the Delhi-based Indian Council of Medical Research and the drug's lead researcher.
But there are some questions over whether this is truly a reversible contraceptive.
Some scientists say Risug is really a replacement for surgical vasectomies, something which the Indian researchers do not entirely deny.
"The contraceptive aspect of the drug still needs to be assessed with expanded reversibility studies. Presently it appears more like a sterilisation approach. The reversibility needed to allow the drug to become a contraceptive needs to be established," Michael Skinner, a reproductive biologist at Washington State University, told me.
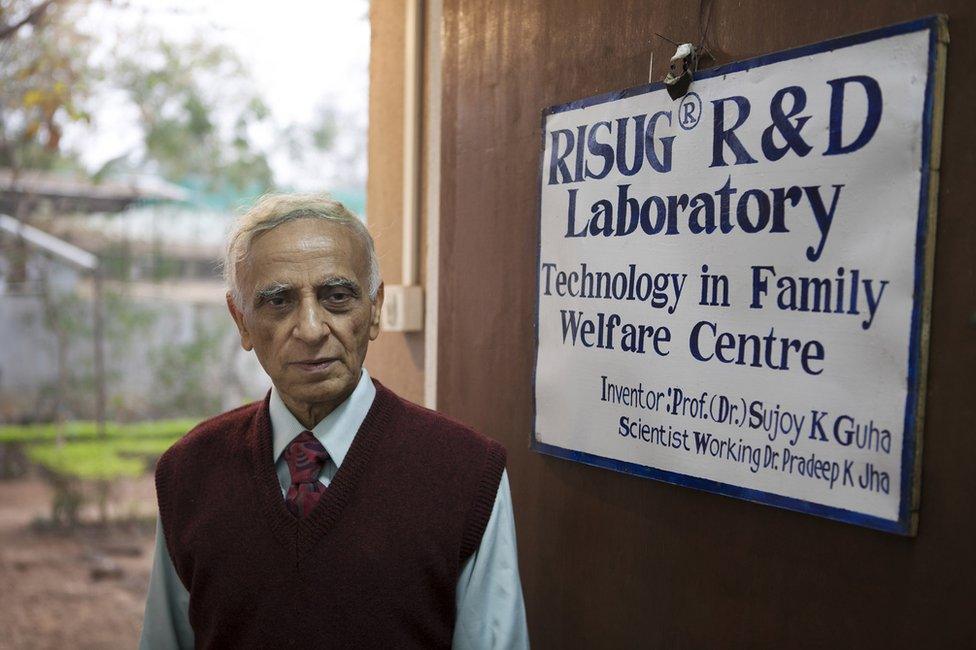
Sujoy Guha has been working on the drug since 1978
Dr Guha agrees. "We are not going to claim reversibility presently, although I am confident that we will be after human trials. For the moment, the drug will be positioned as an improvement on vasectomy. It will cause less trauma to men, and there will be no surgical incision," he says.
Earlier this year Dr Sharma published the results of the clinical trials, external of the drug. Some 139 married men, under the age of 41 and having at least two children, were given a single shot of the injection and monitored for six months.
The wives of 133 of the men did not get pregnant after unprotected sex. The drug's failure to work for six of the men was blamed on "leakage" from the syringe, or the sperm-carrying tubes suffering punctures, according to the results.
But for some researchers like Stephanie Page, professor of medicine at the University of Washington School of Medicine, even this seemingly paltry failure rate is significant. "That may not be any different than scalpel vasectomy in terms of side effects and failure rate. Much more data is needed," Prof Page told me.
On the whole, Prof Page believes the crucial third trial study was "positive", but believes that the number of volunteers (139) was limited and the follow-up period (six months) was "not long by most standards".
"Therefore the drug is a move forward but not a game changer at least for many potential markets," she said.
Indian researchers say Risug has cleared three rounds of human trials - involving more than 500 volunteers since the early 1990s - manufacturing best practices and toxicity tests in the country. Two dozen studies of the drug over three decades are cited to illustrate its efficacy to prevent pregnancy.
The injection will be affordable and a lasting way to prevent pregnancies, they say. They say the volunteers have reported no loss of libido or major side effects. India's drug regulator is expected to green-light the drug soon for production and sale to the public, most likely to be undertaken by the government itself.
It's about time for an effective male birth control option. For decades, women have borne the burden of unplanned pregnancy.
Since pregnancy and childbirth remains dangerous, the imperatives of safe and effective contraception for women have come ahead of the need for male birth control, researchers say. Scientific and social efforts have focussed on female methods.
Nearly 60 years after the first birth control pill became available in the US, women today rely on more than a dozen methods of contraception to prevent unwanted pregnancies: pills and patches; injections and implants; rings and cups; and injections and sponges.
There is substantial international interest in Risug though.

A vasectomy is designed to be permanent, although some men have successfully had the operation reversed
Dr Guha has licensed the drug to a Berkeley-based non-profit, Parsemus Foundation, to launch it in the US, and a related contraceptive called Vasalgel, external is still in pre-clinical trails. Clinical trials of the drug are under way in six European countries. With a grant from the Bill and Melina Gates Foundation, Dr Guha, who also has a doctorate in medical physiology from Missouri's Saint Louis University, has been working on a variant of the drug for women, in which a similar injection into the fallopian tubes will stop pregnancies.
So will men play their part?
In patriarchal societies like India, contraceptive use among men remains low. More than 90% of married couples don't use condoms, according to official data. Male vasectomy rates are pitifully low; and female sterilisation remains a popular contraceptive method.
Researchers believe attitudes might be changing worldwide.
"Time and attitudes are changing globally. One of the reasons men are not as involved in contraception is that they have so few options. The goal of the field is to develop a menu of contraceptives for men; only when that is available will men truly be in a place to share the burden of contraception with their partners," says Dr Page. Time will tell whether Risug will become the breakthrough male birth control urgently needs.
A hormone injection for men has been shown to be 96% effective as contraception.

Read more from Soutik Biswas

Follow Soutik on Twitter at @soutikBBC, external
