How coronavirus is changing NHS technology
- Published

NHS technology is changing at speed, says Adrian Byrne
"Many people within the NHS are talking about two years of transformation done in two weeks," says Adrian Byrne, chief information officer at University Hospital Southampton NHS Foundation Trust (UHSFT).
His hospital has been among the many seeing innovations, including the use of a chatbot to provide automatic alerts for Covid-19 test results.
"Doctors don't look on the system every five minutes to see whether test results are back and this can waste time in being able to discharge or provide patients with care," says Mr Byrne.
The coronavirus outbreak has spurred hospitals to deal with all sorts of technology issues, not least staff having to use devices while dressed in full personal protective equipment (PPE).
At the Queen Elizabeth Hospital in King's Lynn, Dr Peter Young, an anaesthetist and intensive care specialist, had to ask for an app to be built to help non-specialist staff in critical care units to communicate more effectively.
"They continuously have many questions and while in full PPE they have to rely on a number of ad hoc WhatsApp lists to try and track down the right person who can help them or else they physically have to leave the unit to sort out their problem, wasting valuable PPE," he says.
Through the Call 4 Help app, staff can request help from everyone in the ICU through a real-time message board. Senior doctors and nurses can monitor and assign tasks through the app, which has been built with PPE in mind.

Dr Peter Young requested an app to help intensive care staff
"We've made sure it is easy to read through visors, and the onscreen buttons are sensitive enough to work easily through double gloved fingers," says Dr Young.
The iPhone X was chosen for the ICU as it is waterproof for cleaning, has a loud speaker and sensitive microphone. Once the requestor connects with the responder, the app provides a link to switch from the message board to FaceTime or a phone call if required. The app could be rolled out to all NHS hospitals nationwide.
Tech demand
Sarah Wilkinson, NHS Digital's CEO, says that the organisation has had to scale up its NHS 111 service, as it was receiving almost 100 time as much use as before the pandemic.
In addition, NHS Digital has worked with a team at Cambridge University that has built machine learning models to predict the upcoming demand for ICU beds and for ventilators.
This is being extended to estimate how long patients will stay in hospital and eventually, Ms Wilkinson hopes, it could help to simulate the best environments and treatment decisions for patients. These models have been deployed across many NHS trusts already.
The pandemic has also accelerated a number of projects which had been on many NHS trusts' agendas for a very long time.
"The clamour for virtual smart cards instead of physical cards increased as we moved into PPE environments, where putting in the physical card was very difficult," Ms Wilkinson said, explaining that the NHS has rolled out virtual cards as a result.
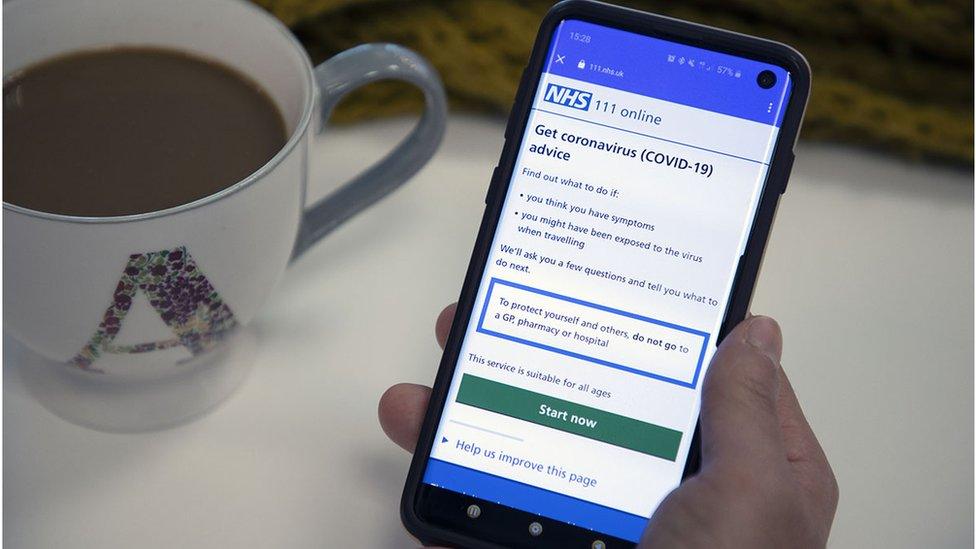
The NHS 111 service has seen a huge rise in demand because of the pandemic
Video conferencing tools had been put on the backburner too, but are now enabling GPs to communicate with patients, doctors to oversee wards and patients to speak to their families and friends.
Mike Ogonovsky, assistant director of informatics at Aneurin Bevan University Health Board says the NHS Wales video consulting service reached 88% of GP practices within a month across Wales, and it has been extended to include hospitals, mental health services and care homes.
"It was an R&D evaluation programme which turned into an aggressive national rollout plan in Wales when the pandemic hit - it became a very black and white issue," he says.
Similar tools are being used across Scotland and England, while Microsoft Teams has been deployed to 1.2 million users with NHS mail.
Another programme of work has been to reduce the amount of paper created in wards.
"If we're creating paper notes in a Covid-19 positive environment then those notes are a risk for 72 hours, so we're placing them somewhere else before scanning them. This is a hassle as the notes are not available immediately and there is a risk to any of the administrative teams who want to go through them," Mr Byrne explains.
One of the biggest frustrations within the NHS is the inability for every organisation to have access to patient details when they're required. Ms Wilkinson says that many of the patient-sharing initiatives that had been built prior to the pandemic, such as GP Connect, have now been commissioned to be made more accessible for Covid-19.


The lingering question then, is why weren't many of these technologies being used prior to the pandemic?
"ICT budgets compete against the budgets of fixing a leaky roof or hiring another clinician, meaning there are immensely difficult judgements to make, particularly as some other costs pay off immediately and IT may be slower to pay off," says Ms Wilkinson.
For instance, some trusts had bought desktop computers instead of laptops because they were cheaper. Even though laptops allow staff to move around more freely and work from home, many trusts may not have believed that this would save money - and all technology projects have to prove that they can save the NHS money to get the green light.
Dr Young says the Call 4 Help app would not have been possible in normal circumstances because of the funds and time required for development. Twenty engineers from Kulestar, 4 Roads, CK Alpha and Concept Softworks have voluntarily worked full-time on the app.
But during this crisis, those in the NHS making the financial decisions have been far more receptive to those on the technology side.
"I think anyone in IT in the NHS would tell you it's been a lot easier to do things in the last few weeks than it would have been prior to the crisis. We're now seeing freeing up of money for digital because it has had to happen," says Mr Byrne.

A SIMPLE GUIDE: How do I protect myself?
IMPACT: What the virus does to the body
RECOVERY: How long does it take?
LOCKDOWN: How can we lift restrictions?
ENDGAME: How do we get out of this mess?

But the NHS may have been in a better place to manage the crisis if certain projects had been given the go-ahead far earlier, says Cindy Fedell, the chief digital and information officer at Bradford Teaching Hospitals NHS Trust.
"Video conferencing is something we could have done one or two years ago, but it was slow to get off the ground, not because of technical issues, but because of people."
Funding is just one part of the problem; there are also strategic and cultural barriers that those in IT in the NHS have to contend with, but Ms Wilkinson believes this will improve as a result of what is now being achieved.
"The art of the possible is so much better understood now, I think we will have a much better understanding [of]... the enormous potential for digitalisation. There will be a broader appetite to invest," she says.