NHS A&E crisis: Staff making 'difficult decisions in unprecedented times'
- Published

The crisis in Britain's A&Es means treating patients in ambulances, a situation which would once have been unthinkable, has become commonplace.
Many hospitals now have staff dedicated to this role, providing not just medical care, but also food and drink.
Meanwhile, hospital corridors have been turned into makeshift wards, filled with patients unable to get a bed in the real wards because they're so full.
The BBC's health correspondent for the North West Gill Dummigan went to Whiston Hospital in Merseyside to see how staff and patients are having to adapt.

The sight hits you as soon as you get through the door of A&E.
Trolley after trolley lined up along the corridor, each one with a patient lying on it and many with anxious relatives standing or sitting patiently next to them.
Nurses go up and down the corridor checking the patients, while others check the bays, which are also full.
All the patients will have spent hours in A&E, and in some cases, days.
Whiston Hospital isn't used to this. It's an outstanding rated trust, one which has always viewed corridor care as an unwelcome exception until now.
Dr Andy Ashton, who has worked as an A&E consultant for 15 years, says they've now had to start including the corridor in their general tracking system.

Dr Andy Ashton is an A&E consultant at the hospital
"We've got little numbers on the wall so we can tell where the patients are," he says.
"We resisted that for a long time, because we didn't want to say that the corridor was actually a place, but we've had to do that.
"I work in a long thin emergency department that used to be called a corridor."
Staff are having to adapt to a different way of working, handing out regular hot meals to A&E patients, and a room is being turned into a temporary kitchen.
There is also an entirely new "ambo" team that has been created to care for the patients who can't even get into the corridors.
Advanced clinical practitioner Sarah McKenna is one of those triaging patients and "bringing A&E to the ambulance".

Sarah McKenna works as an advanced clinical practitioner
"We're giving the exact same care as if they were inside the building... so any blood tests, any X-rays, any treatment they need, toileting, food, drink, everything we would do," she says.
"I'd say we're lucky today that we've managed to get some patients in and some spaces.
"The last couple of days have been particularly trying.
"We've had multiple ambulances out here with patients in for hours on end".
The staff say patients are being kept safe, but no-one's happy about the situation.
Claire Fraser is the senior sister heading the day's "ambo" team.

Claire Fraser, pictured right, says it's not ideal or acceptable
"If you'd have told me 12 months ago, even six months ago, I'd be spending entire shifts out in a car park, I wouldn't have believed you," she says.
"It's not ideal and it's not acceptable, but it's the best that we can do for these patients.
"I think we're all struggling with that".
She says most of the patients are grateful to get treatment and understand the pressures staff are under.
Those who spoke to me praised the medics and said they could see how hard they were working.
Bill Chorlton, who is 75, says they "doing a belting job", adding: "I can't praise them enough, I'll be honest with you."
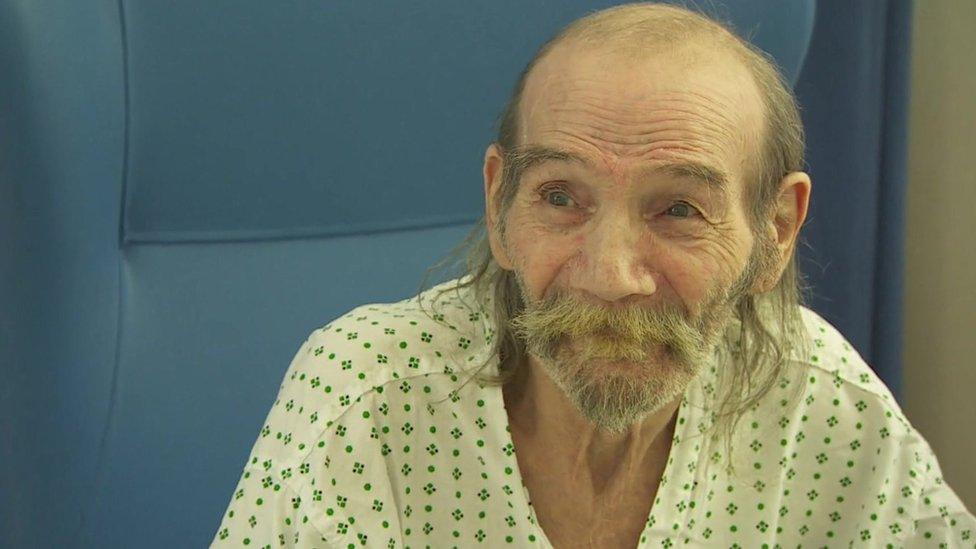
Patient Bill Chorlton heaped praise on hospital staff
When I met Bill, he was in a hospital ward, having spent two weeks being treated for breathing difficulties.
He says the first two days of that was spent in A&E.
"It was [a case of trying to] go to sleep as much as you could, doze off, then you'd wake up [and] you'd be moved up a place," he says.
"It was terrible, horrible, just the waiting and waiting."
Bill is now in a ward which is usually reserved for patients getting hip and knee surgery, but many of those surgical beds are now being used to look after people who are sick.
Professor Rowan Pritchard-Jones is a plastic surgeon at the hospital and medical director for Cheshire and Merseyside.
He says some surgical wards are now two-thirds full of other patients, an exceptionally large number of them with flu.

Professor Rowan Pritchard-Jones says these are "unprecedented times"
"These patients are so poorly, they must come into a surgical ward," he says.
"One of our surgical wards has completely changed into a ward to support flu patients and that inevitably has a knock-on effect for getting operations done."
"We are really sorry for those patients that are having things deferred, because we know they are in pain and struggling at home, but these are the difficult decisions we make in unprecedented times."
Prof Pritchard-Jones says every hospital in the area is struggling to cope, not just with the numbers of A&E patients, but the inability to discharge medically-fit patients because of a lack of social care.
Staff on the orthopaedic ward tell me that of the 20 medical patients there, 14 are ready to go, but there's no care package for them.
Fourteen people is just one short of an entire corridor of patients in A&E.
The feeling here is that the root of much of this crisis is the lack of social care.
Bill is one of those caught up in the system.
He's waiting for a place in respite care and says his rented bungalow has just been declared unfit to live in, because of a rat infestation.
He says he'll be in care until a new home can be found, so "I'm in hospital now not because I'm ill, but because it can't be lived in".
And so it goes on.
While Bill, and the other patients like him, wait for their social care place and the A&E patients wait for a ward bed, the hospital staff battle on, hoping that spring might bring some respite to the situation.

Why not follow BBC North West on Facebook, external, Twitter, external and Instagram, external? You can also send story ideas to northwest.newsonline@bbc.co.uk, external
- Published9 December 2022

- Published8 December 2022

- Published8 December 2022

- Published1 December 2022
