Call to punish GPs over antibiotics
- Published
- comments
Professor Mark Baker, NICE: "People who overuse antibiotics are creating a problem for patients with life-threatening infections"
"Soft-touch" and "hazardous" doctors should be disciplined for prescribing too many antibiotics, a leading NHS figure says.
The National Institute for Health and Care Excellence's Prof Mark Baker said 10 million prescriptions a year in England were inappropriate.
He said regulators need to deal with overprescribing doctors who failed to change their ways.
The Royal College of GPs said the call was "counter-productive and unhelpful".
GP Dr Simon Bowers: "There are people who think the snotty nose they've got needs antibiotics and needs them now"
There is universal consensus that the very basis of modern medicine is under threat due to rising numbers of infections that are resistant to drugs.
The "antibiotic apocalypse" not only means that long-forgotten infections could kill again, but jeopardises procedures including surgery and chemotherapy.
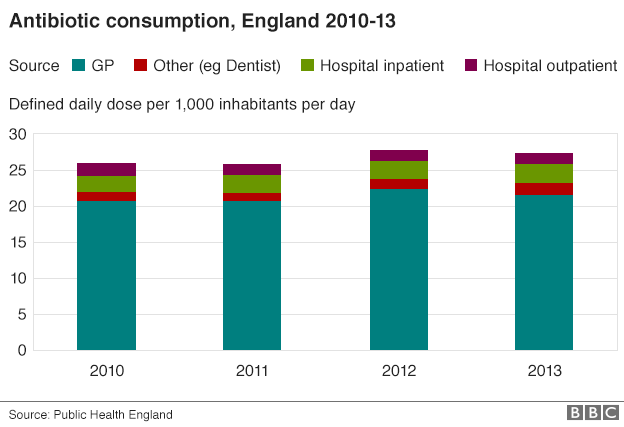
Using antibiotics inappropriately for sore throats and colds increases the risk of resistance. Yet the number of prescriptions continues to rise.

Some bacteria are becoming resistant to our best drugs
NICE has prepared fresh guidelines, external on antibiotic prescribing for the NHS in England, which can be adopted by other parts of the UK.
The guidelines acknowledge that there is huge pressure from some patients for the drugs.

Antibiotics - what are they good for?
Antibiotics can treat bacterial infections, but they are useless against viruses or other types of infection
Colds and most coughs and sore throats are caused by viruses
And our bodies are good at fighting off many common infections, including ear infections, on their own
Your doctor should only prescribe antibiotics when you need them, for example for a kidney infection or pneumonia. Antibiotics may be life-saving for infections such as meningitis
By not using them unnecessarily, they are more likely to work when we need them
You could talk to your pharmacist or GP if you want to learn more

Prof Baker even said some people were "addicted" to the idea of getting antibiotics, even for conditions that would clear up on their own.
He added 97% of patients who asked for antibiotics ended up getting them, often by identifying a "soft-touch" doctor.
The guidelines say doctors should tell patients when antibiotics are inappropriate and refuse to write prescriptions.
Prof Mark Baker, director of the organisation's centre for clinical practice, said: "We are proposing that evidence is collected so the finger can be pointed at people who are a soft touch."
He said antibiotics could cause more harm than good in some patients, so overprescribing was "really hazardous practice".
And, he said, doctors should be encouraged to change their habits. But ultimately some cases should be dealt with by the General Medical Council, which has the power to withdraw a doctor's right to practise, "if necessary".

NICE admits that if previous guidelines on respiratory tract infections, which include colds, were actually followed then prescriptions would be 22% lower.
The latest rules for doctors should cut the 42 million prescriptions given each year by around a quarter.
Dr Tim Ballard, from the Royal College of GPs, said the focus needed to be on "societal change" - not doctors.
He said: "Any suggestion that hard-pressed GPs - who are already trying to do their jobs in increasingly difficult circumstances - will be reported to the regulator is counter-productive and unhelpful."

Case study
Robert, from Dorset, says some doctors are too restrictive.
"My daughter was ill for many weeks because the doctor refused an antibiotic.
"She was very poorly and the doctor said it was just viral and told us to go away. We took her back again and got the same response. We took her for a third time and asked him to test her mucus. He phoned us - rather embarrassed - to say that she had pneumonia.
"He prescribed her antibiotics and she got better quite quickly.
"Weeks of needless suffering!
"I'm sure he was under pressure not to prescribe antibiotics."

NICE will be publishing guidelines on educating the public next year.
Other recommendations include the use of "delayed prescribing" where a patient can only use a prescription if his condition gets worse and creating "antimicrobial stewards" who identify high levels of prescribing.
Niall Dickson, the chief executive of the General Medical Council, said doctors should reflect on their prescribing habits as part of an annual appraisal.
He said "doctors can, and do, face sanctions for mis-prescribing." But the message is "more about changing the norms of practice generally than pursuing individual doctors".
- Published18 August 2015

- Published18 August 2015
- Published18 August 2015

- Published19 November 2015
- Published10 October 2014
- Published14 May 2015
- Published6 April 2015
